
Pfizers tödliche Spritzen
Pfizer bestätigte schon im Februar 2021, was unabhängige Wissenschaftler herausfanden: Der mit einer Notzulassung in einer experimentellen Phase eines Menschenversuches verspritzte Cocktail von vorwiegend unbekannten Substanzen, den wir „Impfstoff“ nennen sollen, macht krank und ist in großer Zahl tödlich. Wie sehr, zeigen die Daten, die Pfizer selbst erstellte und an die Zulassungsbehörden weiterleitete.
Zitat: „Der Bericht wurde erstellt von: Weltweite Sicherheit Pfizer
Die in diesem Dokument enthaltenen Informationen sind urheberrechtlich geschützt und vertraulich. Jegliche Weitergabe, Vervielfältigung, Verteilung oder sonstige Verbreitung dieser Informationen außerhalb von Pfizer, seinen verbundenen Unternehmen, seinen Lizenznehmern oder den Aufsichtsbehörden ist strengstens untersagt. Sofern nicht anderweitig schriftlich vereinbart, verpflichten Sie sich durch die Annahme oder Durchsicht dieser Materialien, diese Informationen vertraulich zu behandeln und sie nicht an andere weiterzugeben (es sei denn, dies ist gesetzlich vorgeschrieben) oder sie für nicht autorisierte Zwecke zu verwenden.“
Wir sehen das anders – wenn milliardenfach experimentelle Substanzen in Menschen gespritzt werden, die sie nicht vor einer vermeintlichen Erkrankung schützen, sie aber in großer Zahl erkranken und sterben lassen, müssen diese Informationen veröffentlicht werden. Es handelt sich um Beweise zur Aufklärung einer globalen Serien von Straftaten.
Die „Nützlichkeits-Ratio“, die Pfizer seinem Giftcocktail vorgeblich unterstellt, ist durch die Wirkungslosigkeit und Schädlichkeit längst widerlegt. Und dennoch wird das Gift weiterhin verspritzt. Auch Kinder sollen damit beschädigt werden und im Herbst kommt noch eine „Impfpflicht“ hinzu. Am Ende des Berichtes finden Sie die Nebenwirkungen (Berichts-Stand 2021) im Einzelnen sowie den Original-Bericht zum Download. Wir halten fest: Alle politischen und wirtschaftlichen Entscheidungsträger hatten Kenntnis von der Gefahr durch die Injektionen. Sie tragen persönlich, aber auch juristisch eine Mitschuld an den verursachten Schäden – einschließlich abertausender Todesfälle. Dieses Dokument wird Teil der Aufarbeitung werden. Es gibt keine Geheimnisse.
Am Ende der Pfizer-Analyse veröffentlicht der Hersteller den Überblick über relevante „Nebenwirkungen“, die berichtet wurden. Kochen Sie sich eine Tasse Tee – es sind einige… eine grobe Übersetzung dieser Nebenwirkungen findet sich ebenfalls als Download am Ende des Berichtes.
5.3.6 CUMULATIVE ANALYSIS OF POST-AUTHORIZATION ADVERSE EVENT REPORTS OF PF-07302048 (BNT162B2) RECEIVED THROUGH 28-FEB-2021
Report Prepared by:
Worldwide Safety Pfizer
The information contained in this document is proprietary and confidential. Any disclosure, reproduction, distribution, or other dissemination of this information outside of Pfizer, its Affiliates, its Licensees, or Regulatory Agencies is strictly prohibited. Except as may be otherwise agreed to in writing, by accepting or reviewing these materials, you agree to hold such information in confidence and not to disclose it to others (except where required by applicable law), nor to use it for unauthorized purposes.
TABLE OF CONTENTS
LIST OF TABLES…………………………………………………………………………………………………….. 3
LIST OF FIGURES……………………………………………………………………………………………………. 3
APPENDICES…………………………………………………………………………………………………………… 3
LIST OF ABBREVIATIONS……………………………………………………………………………………… 4
- INTRODUCTION………………………………………………………………………………………………….. 5
- METHODOLOGY…………………………………………………………………………………………………. 5
- RESULTS……………………………………………………………………………………………………………… 6
- Safety Database…………………………………………………………………………………………… 6
- General Overview……………………………………………………………………………. 6
- Summary of Safety Concerns in the US Pharmacovigilance Plan…………… 9
- Review of Adverse Events of Special Interest (AESIs)……………………….. 16
- Medication error…………………………………………………………………………….. 26
- Safety Database…………………………………………………………………………………………… 6
- DISCUSSION……………………………………………………………………………………………………… 28
- SUMMARY AND CONCLUSION………………………………………………………………………… 29
LIST OF TABLES
Table 1. General Overview: Selected Characteristics of All Cases Received
During the Reporting Interval………………………………………………………….. 7
Table 2. Events Reported in ≥2% Cases………………………………………………………… 8
Table 3. Safety concerns……………………………………………………………………………… 9
Table 4. Important Identified Risk………………………………………………………………. 10
Table 5. Important Potential Risk……………………………………………………………….. 11
Table 6. Description of Missing Information………………………………………………… 12
Table 7. AESIs Evaluation for BNT162b2…………………………………………………… 16
Table 8. ME PTs by seriousness with or without harm co-association
(Through 28 February 2021)………………………………………………………….. 27
LIST OF FIGURES
Figure 1. Total Number of 13vPnC AEs by System Organ Classes and Event Seriousness 8
APPENDICES
APPENDIX 1 LIST OF ADVERSE EVENTS OF SPECIAL INTEREST 30
LIST OF ABBREVIATIONS
| Acronym | Term |
| AE | adverse event |
| AESI | adverse event of special interest |
| BC | Brighton Collaboration |
| CDC | Centers for Disease Control and Prevention |
| COVID-19 | coronavirus disease 2019 |
| DLP | data lock point |
| EUA | emergency use authorisation |
| HLGT | (MedDRA) High Group Level Term |
| HLT | (MedDRA) High Level Term |
| MAH | marketing authorisation holder |
| MedDRA | medical dictionary for regulatory activities |
| MHRA | Medicines and Healthcare products Regulatory Agency |
| PCR | Polymerase Chain Reaction |
| PT | (MedDRA) Preferred Term |
| PVP | pharmacovigilance plan |
| RT-PCR | Reverse Transcription-Polymerase Chain Reaction |
| RSI | reference safety information |
| TME | targeted medically event |
| SARS-CoV-2 | severe acute respiratory syndrome coronavirus 2 |
| SMQ | standardised MedDRA query |
| SOC | (MedDRA) System Organ Class |
| UK | United Kingdom |
| US | United States |
| VAED | vaccine-associated enhanced disease |
| VAERD | vaccine-associated enhanced respiratory disease |
| VAERS | vaccine adverse event reporting system |
1. INTRODUCTION
Reference is made to the Request for Comments and Advice submitted 04 February 2021 regarding Pfizer/BioNTech’s proposal for the clinical and post-authorization safety data package for the Biologics License Application (BLA) for our investigational COVID-19 Vaccine (BNT162b2). Further reference is made to the Agency’s 09 March 2021 response to this request, and specifically, the following request from the Agency.
“Monthly safety reports primarily focus on events that occurred during the reporting interval and include information not relevant to a BLA submission such as line lists of adverse events by country. We are most interested in a cumulative analysis of post-authorization safety data to support your future BLA submission. Please submit an integrated analysis of your cumulative post-authorization safety data, including U.S. and foreign post-authorization experience, in your upcoming BLA submission. Please include a cumulative analysis of the Important Identified Risks, Important Potential Risks, and areas of Important Missing Information identified in your Pharmacovigilance Plan, as well as adverse events of special interest and vaccine administration errors (whether or not associated with an adverse event). Please also include distribution data and an analysis of the most common adverse events. In addition, please submit your updated Pharmacovigilance Plan with your BLA submission.”
This document provides an integrated analysis of the cumulative post-authorization safety data, including U.S. and foreign post-authorization adverse event reports received through 28 February 2021.
2. METHODOLOGY
Pfizer is responsible for the management post-authorization safety data on behalf of the MAH BioNTech according to the Pharmacovigilance Agreement in place. Data from BioNTech are included in the report when applicable.
Pfizer’s safety database contains cases of AEs reported spontaneously to Pfizer, cases reported by the health authorities, cases published in the medical literature, cases from Pfizer-sponsored marketing programs, non-interventional studies, and cases of serious AEs reported from clinical studies regardless of causality assessment.
The limitations of post-marketing adverse drug event reporting should be considered when interpreting these data:
- Reports are submitted voluntarily, and the magnitude of underreporting is unknown. Some of the factors that may influence whether an event is reported include: length of time since marketing, market share of the drug, publicity about a drug or an AE, seriousness of the reaction, regulatory actions, awareness by health professionals and consumers of adverse drug event reporting, and litigation.
- Because many external factors influence whether or not an AE is reported, the spontaneous reporting system yields reporting proportions not incidence rates. As a result, it is generally not appropriate to make between-drug comparisons using these
proportions; the spontaneous reporting system should be used for signal detection rather than hypothesis testing.
- In some reports, clinical information (such as medical history, validation of diagnosis, time from drug use to onset of illness, dose, and use of concomitant drugs) is missing or incomplete, and follow-up information may not be available.
- An accumulation of adverse event reports (AERs) does not necessarily indicate that a particular AE was caused by the drug; rather, the event may be due to an underlying disease or some other factor(s) such as past medical history or concomitant medication.
- Among adverse event reports received into the Pfizer safety database during the cumulative period, only those having a complete workflow cycle in the safety database (meaning they progressed to Distribution or Closed workflow status) are included in the monthly SMSR. This approach prevents the inclusion of cases that are not fully processed hence not accurately reflecting final information. Due to the large numbers of spontaneous adverse event reports received for the product, the MAH has prioritised the processing of serious cases, in order to meet expedited regulatory reporting timelines and ensure these reports are available for signal detection and evaluation activity. The increased volume of reports has not impacted case processing for serious reports, and compliance metrics continue to be monitored weekly with prompt action taken as needed to maintain compliance with expedited reporting obligations. Non-serious cases are entered into the safety database no later than 4 calendar days from receipt. Entrance into the database includes the coding of all adverse events; this allow for a manual review of events being received but may not include immediate case processing to completion.
Non-serious cases are processed as soon as possible and no later than 90 days from receipt. Pfizer has also taken a multiple actions to help alleviate the large increase of adverse event reports. This includes significant technology enhancements, and process and workflow solutions, as well as increasing the number of data entry and case processing colleagues. To date, Pfizer has onboarded approximately (b) (4) additional full- time employees (FTEs). More are joining each month with an expected total of more than (b) (4) additional resources by the end of June 2021.
3. RESULTS
3.1. Safety Database
3.1.1. General Overview
It is estimated that approximately (b) (4) doses of BNT162b2 were shipped worldwide from the receipt of the first temporary authorisation for emergency supply on 01 December 2020 through 28 February 2021.
Cumulatively, through 28 February 2021, there was a total of 42,086 case reports (25,379 medically confirmed and 16,707 non-medically confirmed) containing 158,893 events. Most cases (34,762) were received from United States (13,739), United Kingdom (13,404) Italy (2,578), Germany (1913), France (1506), Portugal (866) and Spain (756); the remaining 7,324 were distributed among 56 other countries.
Table 1 below presents the main characteristics of the overall cases.
Table 1. General Overview: Selected Characteristics of All Cases Received During the Reporting Interval
| Characteristics | Relevant cases (N=42086) | |
| Gender: | Female | 29914 |
| Male | 9182 | |
| No Data | 2990 | |
| Age range (years): | ≤ 17 | 175a |
| 0.01 -107 years | 18-30 | 4953 |
| Mean = 50.9 years | 31-50 | 13886 |
| n = 34952 | 51-64 | 7884 |
| 65-74 | 3098 | |
| ≥ 75 | 5214 | |
| Unknown | 6876 | |
| Case outcome: | Recovered/Recovering | 19582 |
| Recovered with sequelae | 520 | |
| Not recovered at the time of report | 11361 | |
| Fatal | 1223 | |
| Unknown | 9400 |
a. in 46 cases reported age was <16-year-old and in 34 cases <12-year-old.
As shown in Figure 1, the System Organ Classes (SOCs) that contained the greatest number (≥2%) of events, in the overall dataset, were General disorders and administration site conditions (51,335 AEs), Nervous system disorders (25,957), Musculoskeletal and connective tissue disorders (17,283), Gastrointestinal disorders (14,096), Skin and subcutaneous tissue disorders (8,476), Respiratory, thoracic and mediastinal disorders (8,848), Infections and infestations (4,610), Injury, poisoning and procedural complications (5,590), and Investigations (3,693).
Figure 1. Total Number of BNT162b2 AEs by System Organ Classes and Event Seriousness
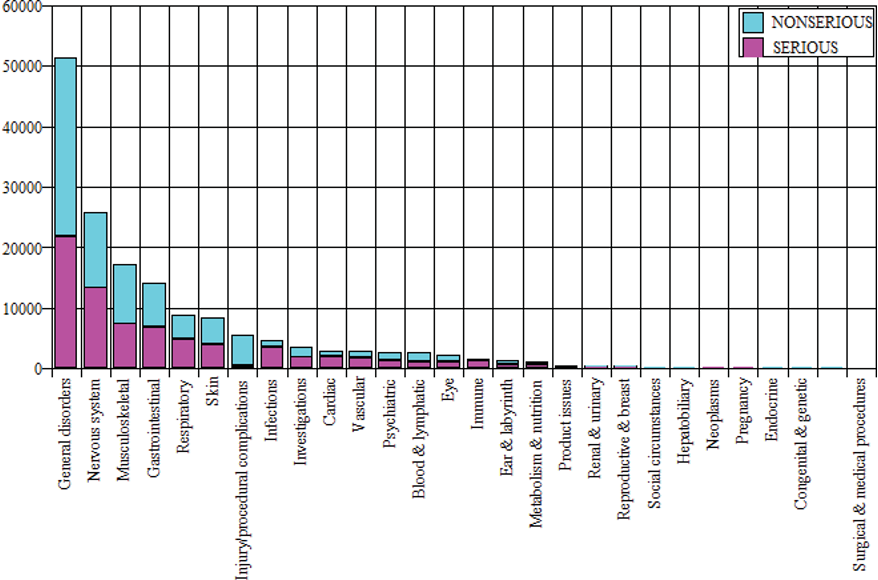
Table 2 shows the most commonly (≥2%) reported MedDRA (v. 23.1) PTs in the overall dataset (through 28 February 2021),
Table 2. Events Reported in ≥2% Cases
| Cumulatively Through 28 February 2021 | ||
| MedDRA SOC | MedDRA PT | AEs (AERP%) N = 42086 |
| Blood and lymphatic system disorders | ||
| Lymphadenopathy | 1972 (4.7%) | |
| Cardiac disorders | ||
| Tachycardia | 1098 (2.6%) | |
| Gastrointestinal disorders | ||
| Nausea | 5182 (12.3%) | |
| Diarrhoea | 1880 (4.5%) | |
| Vomiting | 1698 (4.0%) | |
| General disorders and administration site conditions | ||
| Pyrexia | 7666 (18.2%) | |
| Fatigue | 7338 (17.4%) | |
| Chills | 5514 (13.1%) | |
| Vaccination site pain | 5181 (12.3%) |
Table 2. Events Reported in ≥2% Cases
| Cumulatively Through 28 February 2021 | ||
| MedDRA SOC | MedDRA PT | AEs (AERP%) N = 42086 |
| Pain | 3691 (8.8%) | |
| Malaise | 2897 (6.9%) | |
| Asthenia | 2285 (5.4%) | |
| Drug ineffective | 2201 (5.2%) | |
| Vaccination site erythema | 930 (2.2%) | |
| Vaccination site swelling | 913 (2.2%) | |
| Influenza like illness | 835 (2%) | |
| Infections and infestations | ||
| COVID-19 | 1927 (4.6%) | |
| Injury, poisoning and procedural complications | ||
| Off label use | 880 (2.1%) | |
| Product use issue | 828 (2.0%) | |
| Musculoskeletal and connective tissue disorders | ||
| Myalgia | 4915 (11.7%) | |
| Pain in extremity | 3959 (9.4%) | |
| Arthralgia | 3525 (8.4%) | |
| Nervous system disorders | ||
| Headache | 10131 (24.1%) | |
| Dizziness | 3720 (8.8%) | |
| Paraesthesia | 1500 (3.6%) | |
| Hypoaesthesia | 999 (2.4%) | |
| Respiratory, thoracic and mediastinal disorders | ||
| Dyspnoea | 2057 (4.9%) | |
| Cough | 1146 (2.7%) | |
| Oropharyngeal pain | 948 (2.3%) | |
| Skin and subcutaneous tissue disorders | ||
| Pruritus | 1447 (3.4%) | |
| Rash | 1404 (3.3%) | |
| Erythema | 1044 (2.5%) | |
| Hyperhidrosis | 900 (2.1%) | |
| Urticaria | 862 (2.1%) | |
| Total number of events | 93473 |
3.1.2. Important identified risks Anaphylaxis Important potential risks Vaccine-Associated Enhanced Disease (VAED), Including Vaccine-associated Enhanced Respiratory Disease (VAERD) Missing information Use in Pregnancy and lactation Use in Paediatric Individuals <12 Years of Age Vaccine Effectiveness Summary of Safety Concerns in the US Pharmacovigilance Plan Table 3. Safety concerns
| Brighton Collaboration Level Number of cases BC 1 290 BC 2 311 BC 3 10 BC 4 391 BC 5 831 Total 1833 |
Table 4. Important Identified Risk
| Topic | Description |
| Important Identified Risk | Post Authorization Cases Evaluation (cumulative to 28 Feb 2021) Total Number of Cases in the Reporting Period (N=42086) |
| Anaphylaxis | Since the first temporary authorization for emergency supply under Regulation 174 in the UK (01 December 2020) and through 28 February 2021, 1833 potentially relevant cases were retrieved from the Anaphylactic reaction SMQ (Narrow and Broad) search strategy, applying the MedDRA algorithm. These cases were individually reviewed and assessed according to Brighton Collaboration (BC) definition and level of diagnostic certainty as shown in the Table below: Level 1 indicates a case with the highest level of diagnostic certainty of anaphylaxis, whereas the diagnostic certainty is lowest for Level 3. Level 4 is defined as “reported event of anaphylaxis with insufficient evidence to meet the case definition” and Level 5 as not a case of anaphylaxis. There were 1002 cases (54.0% of the potentially relevant cases retrieved), 2958 potentially relevant events, from the Anaphylactic reaction SMQ (Broad and Narrow) search strategy, meeting BC Level 1 to 4: Country of incidence: UK (261), US (184), Mexico (99), Italy (82), Germany (67), Spain (38), France (36), Portugal (22), Denmark (20), Finland, Greece (19 each), Sweden (17), Czech Republic , Netherlands (16 each), Belgium, Ireland (13 each), Poland (12), Austria (11); the remaining 57 cases originated from 15 different countries. Relevant event seriousness: Serious (2341), Non-Serious (617); Gender: Females (876), Males (106), Unknown (20); Age (n=961) ranged from 16 to 98 years (mean = 54.8 years, median = 42.5 years); Relevant even outcomea: fatal (9)b, resolved/resolving (1922), not resolved (229), resolved with sequelae (48), unknown (754); Most frequently reported relevant PTs (≥2%), from the Anaphylactic reaction SMQ (Broad and Narrow) search strategy: Anaphylactic reaction (435), Dyspnoea (356), Rash (190), Pruritus (175), Erythema (159), Urticaria (133), Cough (115), Respiratory distress, Throat tightness (97 each), Swollen tongue (93), Anaphylactic shock (80), Hypotension (72), Chest discomfort (71), Swelling face (70), Pharyngeal swelling (68), and Lip swelling (64). Conclusion: Evaluation of BC cases Level 1 – 4 did not reveal any significant new safety information. Anaphylaxis is appropriately described in the product labeling as are non-anaphylactic hypersensitivity events. Surveillance will continue. |
a Different clinical outcome may be reported for an event that occurred more than once to the same individual. b There were 4 individuals in the anaphylaxis evaluation who died on the same day they were vaccinated.
Although these patients experienced adverse events (9) that are potential symptoms of anaphylaxis, they all had serious underlying medical conditions, and one individual appeared to also have COVID-19 pneumonia, that likely contributed to their deaths
Table 5. Important Potential Risk
| Topic | Description |
| Important Potential Risk | Post Authorization Cases Evaluation (cumulative to 28 Feb 2021) Total Number of Cases in the Reporting Period (N=42086) |
| Vaccine- Associated Enhanced Disease (VAED), including Vaccine- Associated Enhanced Respiratory Disease (VAERD) | No post-authorized AE reports have been identified as cases of VAED/VAERD, therefore, there is no observed data at this time. An expected rate of VAED is difficult to establish so a meaningful observed/expected analysis cannot be conducted at this point based on available data. The feasibility of conducting such an analysis will be re-evaluated on an ongoing basis as data on the virus grows and the vaccine safety data continues to accrue. The search criteria utilised to identify potential cases of VAED for this report includes PTs indicating a lack of effect of the vaccine and PTs potentially indicative of severe or atypical COVID-19a. Since the first temporary authorization for emergency supply under Regulation 174 in the UK (01 December 2020) and through 28 February 2021, 138 cases [0.33% of the total PM dataset], reporting 317 potentially relevant events were retrieved: |
| Country of incidence: UK (71), US (25), Germany (14), France, Italy, Mexico, Spain, (4 each), Denmark (3); the remaining 9 cases originated from 9 different countries; Cases Seriousness: 138; Seriousness criteria for the total 138 cases: Medically significant (71, of which 8 also serious for disability), Hospitalization required (non-fatal/non-life threatening) (16, of which 1 also serious for disability), Life threatening (13, of which 7 were also serious for hospitalization), Death (38). Gender: Females (73), Males (57), Unknown (8); Age (n=132) ranged from 21 to 100 years (mean = 57.2 years, median = 59.5); Case outcome: fatal (38), resolved/resolving (26), not resolved (65), resolved with sequelae (1), unknown (8); Of the 317 relevant events, the most frequently reported PTs (≥2%) were: Drug ineffective (135), Dyspnoea (53), Diarrhoea (30), COVID-19 pneumonia (23), Vomiting (20), Respiratory failure (8), and Seizure (7). | |
| Conclusion: VAED may present as severe or unusual clinical manifestations of COVID-19. Overall, there were 37 subjects with suspected COVID-19 and 101 subjects with confirmed COVID-19 following one or both doses of the vaccine; 75 of the 101 cases were severe, resulting in hospitalisation, disability, life-threatening consequences or death. None of the 75 cases could be definitively considered as VAED/VAERD. In this review of subjects with COVID-19 following vaccination, based on the current evidence, VAED/VAERD remains a theoretical risk for the vaccine. Surveillance will continue. |
a. Search criteria: Standard Decreased Therapeutic Response Search AND PTs Dyspnoea; Tachypnoea; Hypoxia; COVID 19 pneumonia; Respiratory Failure; Acute Respiratory Distress Syndrome; Cardiac Failure; Cardiogenic shock; Acute myocardial infarction; Arrhythmia; Myocarditis; Vomiting; Diarrhoea; Abdominal pain; Jaundice;
Acute hepatic failure; Deep vein thrombosis; Pulmonary embolism; Peripheral Ischaemia; Vasculitis; Shock; Acute kidney injury; Renal failure; Altered state of consciousness; Seizure; Encephalopathy; Meningitis; Cerebrovascular accident; Thrombocytopenia; Disseminated intravascular coagulation; Chillblains;
Erythema multiforme; Multiple organ dysfunction syndrome; Multisystem inflammatory syndrome in children.
| Topic | Description |
| Missing Information | Post Authorization Cases Evaluation (cumulative to 28 Feb 2021) Total Number of Cases in the Reporting Period (N=42086) |
| Use in Pregnancy and lactation | Number of cases: 413a (0.98% of the total PM dataset); 84 serious and 329 non-serious;Country of incidence: US (205), UK (64), Canada (31), Germany (30), Poland (13), Israel (11); Italy (9), Portugal (8), Mexico (6), Estonia, Hungary and Ireland, (5 each), Romania (4), Spain (3), Czech Republic and France (2 each), the remaining 10 cases were distributed among 10 other countries. Pregnancy cases: 274 cases including: 270 mother cases and 4 foetus/baby cases representing 270 unique pregnancies (the 4 foetus/baby cases were linked to 3 mother cases; 1 mother case involved twins).Pregnancy outcomes for the 270 pregnancies were reported as spontaneous abortion (23), outcome pending (5), premature birth with neonatal death, spontaneous abortion with intrauterine death (2 each), spontaneous abortion with neonatal death, and normal outcome (1 each). No outcome was provided for 238 pregnancies (note that 2 different outcomes were reported for each twin, and both were counted). 146 non-serious mother cases reported exposure to vaccine in utero without the occurrence of any clinical adverse event. The exposure PTs coded to the PTs Maternal exposure during pregnancy (111), Exposure during pregnancy (29) and Maternal exposure timing unspecified (6). Trimester of exposure was reported in 21 of these cases: 1st trimester (15 cases), 2nd trimester (7), and 3rd trimester (2).124 mother cases, 49 non-serious and 75 serious, reported clinical events, which occurred in the vaccinated mothers. Pregnancy related events reported in these cases coded to the PTs Abortion spontaneous (25), Uterine contraction during pregnancy, Premature rupture of membranes, Abortion, Abortion missed, and Foetal death (1 each). Other clinical events which occurred in more than 5 cases coded to the PTs Headache (33), Vaccination site pain (24), Pain in extremity and Fatigue (22 each), Myalgia and Pyrexia (16 each), Chills (13) Nausea (12), Pain (11), Arthralgia (9), Lymphadenopathy and Drug ineffective (7 each), Chest pain, Dizziness and Asthenia (6 each), Malaise and COVID-19 (5 each). Trimester of exposure was reported in 22 of these cases: 1st trimester (19 cases), 2nd trimester (1 case), 3rd trimester (2 cases).4 serious foetus/baby cases reported the PTs Exposure during pregnancy, Foetal growth restriction, Maternal exposure during pregnancy, Premature baby (2 each), and Death neonatal (1). Trimester of exposure was reported for 2 cases (twins) as occurring during the 1st trimester. Breast feeding baby cases: 133, of which: 116 cases reported exposure to vaccine during breastfeeding (PT Exposure via breast milk) without the occurrence of any clinical adverse events;17 cases, 3 serious and 14 non-serious, reported the following clinical events that occurred in the infant/child exposed to vaccine via breastfeeding: Pyrexia (5), Rash (4), Infant irritability (3), Infantile vomiting, Diarrhoea, Insomnia, and Illness (2 each), Poor feeding infant, Lethargy, Abdominal discomfort, Vomiting, Allergy to vaccine, Increased appetite, Anxiety, Crying, Poor quality sleep, Eructation, Agitation, Pain and Urticaria (1 each). Breast feeding mother cases (6): 1 serious case reported 3 clinical events that occurred in a mother during breast feeding (PT Maternal exposure during breast feeding); these events coded to the PTs Chills, Malaise, and Pyrexia1 non-serious case reported with very limited information and without associated AEs. |
| Topic | Description |
| Missing Information | Post Authorization Cases Evaluation (cumulative to 28 Feb 2021) Total Number of Cases in the Reporting Period (N=42086) |
| In 4 cases (3 non-serious; 1 serious) Suppressed lactation occurred in a breast feeding women with the following co-reported events: Pyrexia (2), Paresis, Headache, Chills, Vomiting, Pain in extremity, Arthralgia, Breast pain, Scar pain, Nausea, Migraine, Myalgia, Fatigue and Breast milk discolouration (1 each). Conclusion: There were no safety signals that emerged from the review of these cases of use in pregnancy and while breast feeding. | |
| Use in Paediatric Individuals <12 Years of Age | Paediatric individuals <12 years of age Number of cases: 34d (0.1% of the total PM dataset), indicative of administration in paediatric subjects <12 years of age;Country of incidence: UK (29), US (3), Germany and Andorra (1 each);Cases Seriousness: Serious (24), Non-Serious (10);Gender: Females (25), Males (7), Unknown (2);Age (n=34) ranged from 2 months to 9 years, mean = 3.7 years, median = 4.0;Case outcome: resolved/resolving (16), not resolved (13), and unknown (5).Of the 132 reported events, those reported more than once were as follows: Product administered to patient of inappropriate age (27, see Medication Error), Off label use (11), Pyrexia (6), Product use issue (5), Fatigue, Headache and Nausea (4 each), Vaccination site pain (3), Abdominal pain upper, COVID-19, Facial paralysis, Lymphadenopathy, Malaise, Pruritus and Swelling (2 each). Conclusion: No new significant safety information was identified based on a review of these cases compared with the non-paediatric population. |
| Vaccine Effectiveness | Company conventions for coding cases indicative of lack of efficacy: The coding conventions for lack of efficacy in the context of administration of the COVID-19 vaccine were revised on 15 February 2021, as shown below: PT “Vaccination failure” is coded when ALL of the following criteria are met:The subject has received the series of two doses per the dosing regimen in local labeling.At least 7 days have elapsed since the second dose of vaccine has been administered.The subject experiences SARS-CoV-2 infection (confirmed laboratory tests).PT “Drug ineffective” is coded when either of the following applies:The infection is not confirmed as SARS-CoV-2 through laboratory tests (irrespective of the vaccination schedule). This includes scenarios where LOE is stated or implied, e.g., “the vaccine did not work”, “I got COVID-19”.It is unknown:Whether the subject has received the series of two doses per the dosing regimen in local labeling;How many days have passed since the first dose (including unspecified number of days like” a few days”, “some days”, etc.);If 7 days have passed since the second dose;The subject experiences a vaccine preventable illness 14 days after receiving the first dose up to and through 6 days after receipt of the second dose. Note: after the immune system as had sufficient time (14 days) to respond to the vaccine, a report of COVID-19 is considered a potential lack of efficacy even if the vaccination course is not complete. Summary of the coding conventions for onset of vaccine preventable disease versus the vaccination date: |
| Topic | Description | ||||
| Missing Information | Post Authorization Cases Evaluation (cumulative to 28 Feb 2021) Total Number of Cases in the Reporting Period (N=42086) | ||||
| 1st dose (day 1-13) | From day 14 post 1st dose to day 6 post 2nd dose | Day 7 post 2nd dose | |||
| Code only the events describing the SARS-CoV-2 infection | Code “Drug ineffective” | Code “Vaccination failure” | |||
| Scenario Not considered LOE | Scenario considered LOE as “Drug ineffective” | Scenario considered LOE as “Vaccination failure” | |||
| Lack of efficacy cases Number of cases: 1665b (3.9 % of the total PM dataset) of which 1100 were medically confirmed and 565 non medically confirmed;Number of lack of efficacy events: 1665 [PT: Drug ineffective (1646) and Vaccination failure (19)f].Country of incidence: US (665), UK (405), Germany (181), France (85), Italy (58), Romania (47), Belgium (33), Israel (30), Poland (28), Spain (21), Austria (18), Portugal (17), Greece (15), Mexico (13), Denmark (8), Canada (7), Hungary, Sweden and United Arab Emirates (5 each), Czech Republic (4), Switzerland (3); the remaining 12 cases originated from 9 different countries.COVID-19 infection was suspected in 155 cases, confirmed in 228 cases, in 1 case it was reported that the first dose was not effective (no other information).COVID-19 infection (suspected or confirmed) outcome was reported as resolved/resolving (165), not resolved (205) or unknown (1230) at the time of the reporting; there were 65 cases where a fatal outcome was reported. Drug ineffective cases (1649) Drug ineffective event seriousness: serious (1625), non-serious (21)e;Lack of efficacy term was reported:after the 1st dose in 788 casesafter the 2nd dose in 139 casesin 722 cases it was unknown after which dose the lack of efficacy occurred.Latency of lack of efficacy term reported after the first dose was known for 176 cases:Within 9 days: 2 subjects;Within 14 and 21 days: 154 subjects;Within 22 and 50 days: 20 subjects;Latency of lack of efficacy term reported after the second dose was known for 69 cases:Within 0 and 7 days: 42 subjects;Within 8 and 21 days: 22 subjects;Within 23 and 36 days: 5 subjects.Latency of lack of efficacy term reported in cases where the number of doses administered was not provided, was known in 409 cases:Within 0 and 7 days after vaccination: 281 subjects.Within 8 and 14 days after vaccination: 89 subjects.Within 15 and 44 days after vaccination: 39 subjects. According to the RSI, individuals may not be fully protected until 7 days after their second dose of vaccine, therefore for the above 1649 cases where lack of efficacy was reported after the 1st dose or the |
| Topic | Description |
| Missing Information | Post Authorization Cases Evaluation (cumulative to 28 Feb 2021) Total Number of Cases in the Reporting Period (N=42086) |
| 2nd dose, the reported events may represent signs and symptoms of intercurrent or undiagnosed COVID- 19 infection or infection in an individual who was not fully vaccinated, rather than vaccine ineffectiveness. Vaccination failure cases (16) Vaccination failure seriousness: all serious;Lack of efficacy term was reported in all cases after the 2nd dose:Latency of lack of efficacy was known for 14 cases:Within 7 and 13 days: 8 subjects;Within 15 and 29 days: 6 subjects. COVID-19 (10) and Asymptomatic COVID-19 (6) were the reported vaccine preventable infections that occurred in these 16 cases. Conclusion: No new safety signals of vaccine lack of efficacy have emerged based on a review of these cases. |
- From a total of 417 cases, 4 cases were excluded from the analysis. In 3 cases, the MAH was informed that a 33-year-old and two unspecified age pregnant female patients were scheduled to receive bnt162b2 (PT reported Off label use and Product use issue in 2 cases; Circumstance or information capable of leading to medication error in one case). One case reported the PT Morning sickness; however, pregnancy was not confirmed in this case.
- 558 additional cases retrieved in this dataset were excluded from the analysis; upon review, 546 cases cannot be considered true lack of efficacy cases because the PT Drug ineffective was coded but the subjects developed SARS-CoV-2 infection during the early days from the first dose (days 1 – 13); the vaccine has not had sufficient time to stimulate the immune system and, consequently, the development of a vaccine preventable disease during this time is not considered a potential lack of effect of the vaccine; in 5 cases the PT Drug ineffective was removed after data lock point (DLP) because the subjects did not develop COVID- 19 infection; in 1 case, reporting Treatment failure and Transient ischaemic attack, the Lack of efficacy PT did not refer to BNT162b2 vaccine; 5 cases have been invalidated in the safety database after DLP; 1 case has been deleted from the discussion because the PTs reported Pathogen resistance and Product preparation issue were not indicative of a lack of efficacy. to be eliminated.
- Upon review, 31 additional cases were excluded from the analysis as the data reported (e.g. clinical details, height, weight, etc.) were not consistent with paediatric subjects
- Upon review, 28 additional cases were excluded from the analysis as the data reported (e.g. clinical details, height, weight, etc.) were not consistent with paediatric subjects.
- Different clinical outcomes may be reported for an event that occurred more than once to the same individual
- In 2 cases the PT Vaccination failure was replaced with Drug ineffective after DLP. Another case was not included in the discussion of the Vaccination failure cases because correct scheduling (21 days apart between the first and second dose) cannot be confirmed.
3.1.3. Review of Adverse Events of Special Interest (AESIs)
Please refer to Appendix 1 for the list of the company’s AESIs for BNT162b2.
The company’s AESI list takes into consideration the lists of AESIs from the following expert groups and regulatory authorities: Brighton Collaboration (SPEAC), ACCESS protocol, US CDC (preliminary list of AESI for VAERS surveillance), MHRA (unpublished guideline).
The AESI terms are incorporated into a TME list and include events of interest due to their association with severe COVID-19 and events of interest for vaccines in general.
The AESI list is comprised of MedDRA PTs, HLTs, HLGTs or MedDRA SMQs and can be changed as appropriate based on the evolving safety profile of the vaccine.
Table 7 provides a summary review of cumulative cases within AESI categories in the Pfizer safety database. This is distinct from safety signal evaluations which are conducted and included, as appropriate, in the Summary Monthly Safety Reports submitted regularly to the FDA and other Health Authorities.
Table 7. AESIs Evaluation for BNT162b2
| AESIsa Category | Post-Marketing Cases Evaluationb Total Number of Cases (N=42086) |
| Anaphylactic Reactions Search criteria: Anaphylactic reaction SMQ (Narrow and Broad, with the algorithm applied), selecting relevant cases according to BC criteria | Please refer to the Risk ‘Anaphylaxis’ included above in Table 4. |
| Cardiovascular AESIs Search criteria: PTs Acute myocardial infarction; Arrhythmia; Cardiac failure; Cardiac failure acute; Cardiogenic shock; Coronary artery disease; Myocardial infarction; Postural orthostatic tachycardia syndrome; Stress cardiomyopathy; Tachycardia | Number of cases: 1403 (3.3% of the total PM dataset), of which 241 are medically confirmed and 1162 are non-medically confirmed;Country of incidence: UK (268), US (233), Mexico (196), Italy (141), France (128), Germany (102), Spain (46), Greece (45), Portugal (37), Sweden (20), Ireland (17), Poland (16), Israel (13), Austria, Romania and Finland (12 each), Netherlands (11), Belgium and Norway (10 each), Czech Republic (9), Hungary and Canada (8 each), Croatia and Denmark (7 each), Iceland (5); the remaining 30 cases were distributed among 13 other countries;Subjects’ gender: female (1076), male (291) and unknown (36);Subjects’ age group (n = 1346): Adultc (1078), Elderlyd (266) Childe and Adolescentf (1 each);Number of relevant events: 1441, of which 946 serious, 495 non-serious; in the cases reporting relevant serious events;Reported relevant PTs: Tachycardia (1098), Arrhythmia (102), Myocardial infarction (89), Cardiac failure (80), Acute myocardial infarction (41), Cardiac failure acute (11), Cardiogenic shock and Postural orthostatic tachycardia syndrome (7 each) and Coronary artery disease (6);Relevant event onset latency (n = 1209): Range from <24 hours to 21 days, median <24 hours; |
| AESIsa Category | Post-Marketing Cases Evaluationb Total Number of Cases (N=42086) |
| Relevant event outcomeg: fatal (136), resolved/resolving (767), resolved with sequelae (21), not resolved (140) and unknown (380); Conclusion: This cumulative case review does not raise new safety issues. Surveillance will continue | |
| COVID-19 AESIs Search criteria: Covid-19 SMQ (Narrow and Broad) OR PTs Ageusia; Anosmia | Number of cases: 3067 (7.3% of the total PM dataset), of which 1013 are medically confirmed and 2054 are non-medically confirmed;Country of incidence: US (1272), UK (609), Germany (360), France (161), Italy (94), Spain (69), Romania (62), Portugal (51), Poland (50), Mexico (43), Belgium (42), Israel (41), Sweden (30), Austria (27), Greece (24), Denmark (18), Czech Republic and Hungary (17 each), Canada (12), Ireland (11), Slovakia (9), Latvia and United Arab Emirates (6 each); the remaining 36 cases were distributed among 16 other different countries;Subjects’ gender: female (1650), male (844) and unknown (573);Subjects’ age group (n= 1880): Adult (1315), Elderly (560), Infanth and Adolescent (2 each), Child (1);Number of relevant events: 3359, of which 2585 serious, 774 non-serious;Most frequently reported relevant PTs (>1 occurrence): COVID- 19 (1927), SARS-CoV-2 test positive (415), Suspected COVID-19 (270), Ageusia (228), Anosmia (194), SARS-CoV-2 antibody test negative (83), Exposure to SARS-CoV-2 (62), SARS-CoV-2 antibody test positive (53), COVID-19 pneumonia (51), Asymptomatic COVID-19 (31), Coronavirus infection (13), Occupational exposure to SARS-CoV-2 (11), SARS-CoV-2 test false positive (7), Coronavirus test positive (6), SARS-CoV-2 test negative (3) SARS-CoV-2 antibody test (2);Relevant event onset latency (n = 2070): Range from <24 hours to 374 days, median 5 days;Relevant event outcome: fatal (136), not resolved (547), resolved/resolving (558), resolved with sequelae (9) and unknown (2110). Conclusion: This cumulative case review does not raise new safety issues. Surveillance will continue |
| Dermatological AESIs Search criteria: PT Chillblains; Erythema multiforme | Number of cases: 20 cases (0.05% of the total PM dataset), of which 15 are medically confirmed and 5 are non-medically confirmed;Country of incidence: UK (8), France and Poland (2 each), and the remaining 8 cases were distributed among 8 other different countries;Subjects’ gender: female (17) male and unknown (1 each);Subjects’ age group (n=19): Adult (18), Elderly (1);Number of relevant events: 20 events, 16 serious, 4 non-serious |
| AESIsa Category | Post-Marketing Cases Evaluationb Total Number of Cases (N=42086) |
| Reported relevant PTs: Erythema multiforme (13) and Chillblains (7)Relevant event onset latency (n = 18): Range from <24 hours to 17 days, median 3 days;Relevant event outcome: resolved/resolving (7), not resolved (8) and unknown (6). Conclusion: This cumulative case review does not raise new safety issues. Surveillance will continue. | |
| Haematological AESIs Search criteria: Leukopenias NEC (HLT) (Primary Path) OR Neutropenias (HLT) (Primary Path) OR PTs Immune thrombocytopenia, Thrombocytopenia OR SMQ Haemorrhage terms (excl laboratory terms | Number of cases: 932 (2.2 % of the total PM dataset), of which 524 medically confirmed and 408 non-medically confirmed;Country of incidence: UK (343), US (308), France (50), Germany (43), Italy (37), Spain (27), Mexico and Poland (13 each), Sweden (10), Israel (9), Netherlands (8), Denmark, Finland, Portugal and Ireland (7 each), Austria and Norway (6 each), Croatia (4), Greece, Belgium, Hungary and Switzerland (3 each), Cyprus, Latvia and Serbia (2 each); the remaining 9 cases originated from 9 different countries;Subjects’ gender (n=898): female (676) and male (222);Subjects’ age group (n=837): Adult (543), Elderly (293), Infant (1);Number of relevant events: 1080, of which 681 serious, 399 non-serious;Most frequently reported relevant PTs (≥15 occurrences) include: Epistaxis (127), Contusion (112), Vaccination site bruising (96), Vaccination site haemorrhage (51), Petechiae (50), Haemorrhage (42), Haematochezia (34), Thrombocytopenia (33), Vaccination site haematoma (32), Conjunctival haemorrhage and Vaginal haemorrhage (29 each), Haematoma, Haemoptysis and Menorrhagia (27 each), Haematemesis (25), Eye haemorrhage (23), Rectal haemorrhage (22), Immune thrombocytopenia (20), Blood urine present (19), Haematuria, Neutropenia and Purpura (16 each) Diarrhoea haemorrhagic (15);Relevant event onset latency (n = 787): Range from <24 hours to 33 days, median = 1 day;Relevant event outcome: fatal (34), resolved/resolving (393), resolved with sequelae (17), not resolved (267) and unknown (371). Conclusion: This cumulative case review does not raise new safety issues. Surveillance will continue |
| Hepatic AESIs Search criteria: Liver related investigations, signs and symptoms (SMQ) (Narrow and Broad) OR PT Liver injury | Number of cases: 70 cases (0.2% of the total PM dataset), of which 54 medically confirmed and 16 non-medically confirmed;Country of incidence: UK (19), US (14), France (7), Italy (5), Germany (4), Belgium, Mexico and Spain (3 each), Austria, and Iceland (2 each); the remaining 8 cases originated from 8 different countries;Subjects’ gender: female (43), male (26) and unknown (1);Subjects’ age group (n=64): Adult (37), Elderly (27); |
| AESIsa Category | Post-Marketing Cases Evaluationb Total Number of Cases (N=42086) |
| Number of relevant events: 94, of which 53 serious, 41 non-serious;Most frequently reported relevant PTs (≥3 occurrences) include: Alanine aminotransferase increased (16), Transaminases increased and Hepatic pain (9 each), Liver function test increased (8), Aspartate aminotransferase increased and Liver function test abnormal (7 each), Gamma-glutamyltransferase increased and Hepatic enzyme increased (6 each), Blood alkaline phosphatase increased and Liver injury (5 each), Ascites, Blood bilirubin increased and Hypertransaminasaemia (3 each);Relevant event onset latency (n = 57): Range from <24 hours to 20 days, median 3 days;Relevant event outcome: fatal (5), resolved/resolving (27), resolved with sequelae (1), not resolved (14) and unknown (47). Conclusion: This cumulative case review does not raise new safety issues. Surveillance will continue | |
| Facial Paralysis Search criteria: PTs Facial paralysis, Facial paresis | Number of cases: 449i (1.07% of the total PM dataset), 314 medically confirmed and 135 non-medically confirmed;Country of incidence: US (124), UK (119), Italy (40), France (27), Israel (20), Spain (18), Germany (13), Sweden (11), Ireland (9), Cyprus (8), Austria (7), Finland and Portugal (6 each), Hungary and Romania (5 each), Croatia and Mexico (4 each), Canada (3),Czech Republic, Malta, Netherlands, Norway, Poland and Puerto Rico (2 each); the remaining 8 cases originated from 8 different countries;Subjects’ gender: female (295), male (133), unknown (21);Subjects’ age group (n=411): Adult (313), Elderly (96), Infantj and Child (1 each);Number of relevant eventsk: 453, of which 399 serious, 54 non-serious;Reported relevant PTs: Facial paralysis (401), Facial paresis (64);Relevant event onset latency (n = 404): Range from <24 hours to 46 days, median 2 days;Relevant event outcome: resolved/resolving (184), resolved with sequelae (3), not resolved (183) and unknown (97); Overall Conclusion: This cumulative case review does not raise new safety issues. Surveillance will continue. Causality assessment will be further evaluated following availability of additional unblinded data from the clinical study C4591001, which will be unblinded for final analysis approximately mid-April 2021. Additionally, non- interventional post-authorisation safety studies, C4591011 and C4591012 are expected to capture data on a sufficiently large vaccinated population to detect an increased risk of Bell’s palsy in vaccinated individuals. The timeline for conducting these analyses will be established based on the size of the vaccinated population captured in the study data sources by the first interim reports (due 30 June |
| AESIsa Category | Post-Marketing Cases Evaluationb Total Number of Cases (N=42086) |
| 2021). Study C4591021, pending protocol endorsement by EMA, is also intended to inform this risk. | |
| Immune-Mediated/Autoimmune AESIs Search criteria: Immune- mediated/autoimmune disorders (SMQ) (Broad and Narrow) OR Autoimmune disorders HLGT (Primary Path) OR PTs Cytokine release syndrome; Cytokine storm; Hypersensitivity | Number of cases: 1050 (2.5 % of the total PM dataset), of which 760 medically confirmed and 290 non-medically confirmed;Country of incidence (>10 cases): UK (267), US (257), Italy (70), France and Germany (69 each), Mexico (36), Sweden (35), Spain (32), Greece (31), Israel (21), Denmark (18), Portugal (17), Austria and Czech Republic (16 each), Canada (12), Finland (10). The remaining 74 cases were from 24 different countries.Subjects’ gender (n=682): female (526), male (156).Subjects’ age group (n=944): Adult (746), Elderly (196), Adolescent (2).Number of relevant events: 1077, of which 780 serious, 297 non‑serious.Most frequently reported relevant PTs (>10 occurrences): Hypersensitivity (596), Neuropathy peripheral (49), Pericarditis (32), Myocarditis (25), Dermatitis (24), Diabetes mellitus and Encephalitis (16 each), Psoriasis (14), Dermatitis Bullous (13), Autoimmune disorder and Raynaud’s phenomenon (11 each);Relevant event onset latency (n = 807): Range from <24 hours to 30 days, median <24 hours.Relevant event outcomel: resolved/resolving (517), not resolved (215), fatal (12), resolved with sequelae (22) and unknown (312). Conclusion: This cumulative case review does not raise new safety issues. Surveillance will continue |
| Musculoskeletal AESIs Search criteria: PTs Arthralgia; Arthritis; Arthritis bacterialn; Chronic fatigue syndrome; Polyarthritis; Polyneuropathy; Post viral fatigue syndrome; Rheumatoid arthritis | Number of cases: 3600 (8.5% of the total PM dataset), of which 2045 medically confirmed and 1555 non-medically confirmed;Country of incidence: UK (1406), US (1004), Italy (285), Mexico (236), Germany (72), Portugal (70), France (48), Greece and Poland (46), Latvia (33), Czech Republic (32), Israel and Spain (26), Sweden (25), Romania (24), Denmark (23), Finland and Ireland (19 each), Austria and Belgium (18 each), Canada (16), Netherlands (14), Bulgaria (12), Croatia and Serbia (9 each), Cyprus and Hungary (8 each), Norway (7), Estonia and Puerto Rico (6 each), Iceland and Lithuania (4 each); the remaining 21 cases originated from 11 different countries;Subjects’ gender (n=3471): female (2760), male (711);Subjects’ age group (n=3372): Adult (2850), Elderly (515), Child (4), Adolescent (2), Infant (1);Number of relevant events: 3640, of which 1614 serious, 2026 non-serious;Reported relevant PTs: Arthralgia (3525), Arthritis (70), Rheumatoid arthritis (26), Polyarthritis (5), Polyneuropathy, Post viral fatigue syndrome, Chronic fatigue syndrome (4 each), Arthritis bacterial (1);Relevant event onset latency (n = 2968): Range from <24 hours to 32 days, median 1 day; |
| AESIsa Category | Post-Marketing Cases Evaluationb Total Number of Cases (N=42086) |
| Relevant event outcome: resolved/resolving (1801), not resolved (959), resolved with sequelae (49), and unknown (853). Conclusion: This cumulative case review does not raise new safety issues. Surveillance will continue. | |
| Neurological AESIs (including demyelination) Search criteria: Convulsions (SMQ) (Broad and Narrow) OR Demyelination (SMQ) (Broad and Narrow) OR PTs Ataxia; Cataplexy; Encephalopathy; Fibromyalgia; Intracranial pressure increased; Meningitis; Meningitis aseptic; Narcolepsy | Number of cases: 501 (1.2% of the total PM dataset), of which 365 medically confirmed and 136 non-medically confirmed.Country of incidence (≥9 cases): UK (157), US (68), Germany (49), Mexico (35), Italy (31), France (25), Spain (18), Poland (17), Netherlands and Israel (15 each), Sweden (9). The remaining 71 cases were from 22 different countries.Subjects’ gender (n=478): female (328), male (150).Subjects’ age group (n=478): Adult (329), Elderly (149);Number of relevant events: 542, of which 515 serious, 27 non‑serious.Most frequently reported relevant PTs (˃2 occurrences) included: Seizure (204), Epilepsy (83), Generalised tonic-clonic seizure (33), Guillain-Barre syndrome (24), Fibromyalgia and Trigeminal neuralgia (17 each), Febrile convulsion, (15), Status epilepticus (12), Aura and Myelitis transverse (11 each), Multiple sclerosis relapse and Optic neuritis (10 each), Petit mal epilepsy and Tonic convulsion (9 each), Ataxia (8), Encephalopathy and Tonic clonic movements (7 each), Foaming at mouth (5), Multiple sclerosis, Narcolepsy and Partial seizures (4 each), Bad sensation, Demyelination, Meningitis, Postictal state, Seizure like phenomena and Tongue biting (3 each);Relevant event onset latency (n = 423): Range from <24 hours to 48 days, median 1 day;Relevant events outcome: fatal (16), resolved/resolving (265), resolved with sequelae (13), not resolved (89) and unknown (161); Conclusion: This cumulative case review does not raise new safety issues. Surveillance will continue |
| Other AESIs Search criteria: Herpes viral infections (HLT) (Primary Path) OR PTs Adverse event following immunisation; Inflammation; Manufacturing laboratory analytical testing issue; Manufacturing materials issue; Manufacturing production issue; MERS-CoV test; MERS-CoV test negative; MERS-CoV test positive; Middle East respiratory syndrome; Multiple organ dysfunction syndrome; Occupational exposure to communicable disease; Patient | Number of cases: 8152 (19.4% of the total PM dataset), of which 4977 were medically confirmed and 3175 non-medically confirmed;Country of incidence (> 20 occurrences): UK (2715), US (2421), Italy (710), Mexico (223), Portugal (210), Germany (207), France (186), Spain (183), Sweden (133), Denmark (127), Poland (120), Greece (95), Israel (79), Czech Republic (76), Romania (57), Hungary (53), Finland (52), Norway (51), Latvia (49), Austria (47), Croatia (42), Belgium (41), Canada (39), Ireland (34), Serbia (28), Iceland (25), Netherlands (22). The remaining 127 cases were from 21 different countries;Subjects’ gender (n=7829): female (5969), male (1860);Subjects’ age group (n=7479): Adult (6330), Elderly (1125), Adolescent, Child (9 each), Infant (6); |
| AESIsa Category | Post-Marketing Cases Evaluationb Total Number of Cases (N=42086) |
| isolation; Product availability issue; Product distribution issue; Product supply issue; Pyrexia; Quarantine; SARS-CoV-1 test; SARS-CoV-1 test negative; SARS- CoV-1 test positive | Number of relevant events: 8241, of which 3674 serious, 4568 non‑serious;Most frequently reported relevant PTs (≥6 occurrences) included: Pyrexia (7666), Herpes zoster (259), Inflammation (132), Oral herpes (80), Multiple organ dysfunction syndrome (18), Herpes virus infection (17), Herpes simplex (13), Ophthalmic herpes zoster (10), Herpes ophthalmic and Herpes zoster reactivation (6 each);Relevant event onset latency (n =6836): Range from <24 hours to 61 days, median 1 day;Relevant events outcome: fatal (96), resolved/resolving (5008), resolved with sequelae (84), not resolved (1429) and unknown (1685). Conclusion: This cumulative case review does not raise new safety issues. Surveillance will continue |
| Pregnancy Related AESIs Search criteria: PTs Amniotic cavity infection; Caesarean section; Congenital anomaly; Death neonatal; Eclampsia; Foetal distress syndrome; Low birth weight baby; Maternal exposure during pregnancy; Placenta praevia; Pre-eclampsia; Premature labour; Stillbirth; Uterine rupture; Vasa praevia | For relevant cases, please refer to Table 6, Description of Missing Information, Use in Pregnancy and While Breast Feeding |
| Renal AESIs Search criteria: PTs Acute kidney injury; Renal failure. | Number of cases: 69 cases (0.17% of the total PM dataset), of which 57 medically confirmed, 12 non-medically confirmed;Country of incidence: Germany (17), France and UK (13 each), US (6), Belgium, Italy and Spain (4 each), Sweden (2), Austria, Canada, Denmark, Finland, Luxembourg and Norway (1 each);Subjects’ gender: female (46), male (23);Subjects’ age group (n=68): Adult (7), Elderly (60), Infant (1);Number of relevant events: 70, all serious;Reported relevant PTs: Acute kidney injury (40) and Renal failure (30);Relevant event onset latency (n = 42): Range from <24 hours to 15 days, median 4 days;Relevant event outcome: fatal (23), resolved/resolving (10), not resolved (15) and unknown (22). Conclusion: This cumulative case review does not raise new safety issues. Surveillance will continue. |
| Respiratory AESIs Search criteria: Lower respiratory tract infections NEC (HLT) | Number of cases: 130 cases (0.3% of the total PM dataset), of which 107 medically confirmed; |
| AESIsa Category | Post-Marketing Cases Evaluationb Total Number of Cases (N=42086) |
| (Primary Path) OR Respiratory failures (excl neonatal) (HLT) (Primary Path) OR Viral lower respiratory tract infections (HLT) (Primary Path) OR PTs: Acute respiratory distress syndrome; Endotracheal intubation; Hypoxia; Pulmonary haemorrhage; Respiratory disorder; Severe acute respiratory syndrome | Countries of incidence: United Kingdom (20), France (18), United States (16), Germany (14), Spain (13), Belgium and Italy (9), Denmark (8), Norway (5), Czech Republic, Iceland (3 each); the remaining 12 cases originated from 8 different countries.Subjects’ gender (n=130): female (72), male (58).Subjects’s age group (n=126): Elderly (78), Adult (47), Adolescent (1).Number of relevant events: 137, of which 126 serious, 11 non-serious;Reported relevant PTs: Respiratory failure (44), Hypoxia (42), Respiratory disorder (36), Acute respiratory distress syndrome (10), Chronic respiratory syndrome (3), Severe acute respiratory syndrome (2).Relevant event onset latency (n=102): range from < 24 hours to 18 days, median 1 day;Relevant events outcome: fatal (41), Resolved/resolving (47), not recovered (18) and unknown (31). Conclusion: This cumulative case review does not raise new safety issues. Surveillance will continue. |
| Thromboembolic Events Search criteria: Embolism and thrombosis (HLGT) (Primary Path), excluding PTs reviewed as Stroke AESIs, OR PTs Deep vein thrombosis; Disseminated intravascular coagulation; Embolism; Embolism venous; Pulmonary embolism | Number of cases: 151 (0.3% of the total PM dataset), of which 111 medically confirmed and 40 non-medically confirmed;Country of incidence: UK (34), US (31), France (20), Germany (15), Italy and Spain (6 each), Denmark and Sweden (5 each), Austria, Belgium and Israel (3 each), Canada, Cyprus, Netherlands and Portugal (2 each); the remaining 12 cases originated from 12 different countries;Subjects’ gender (n= 144): female (89), male (55);Subjects’ age group (n=136): Adult (66), Elderly (70);Number of relevant events: 168, of which 165 serious, 3 non-serious;Most frequently reported relevant PTs (>1 occurrence) included: Pulmonary embolism (60), Thrombosis (39), Deep vein thrombosis (35), Thrombophlebitis superficial (6), Venous thrombosis limb (4), Embolism, Microembolism, Thrombophlebitis and Venous thrombosis (3 each) Blue toe syndrome (2);Relevant event onset latency (n = 124): Range from <24 hours to 28 days, median 4 days;Relevant event outcome: fatal (18), resolved/resolving (54), resolved with sequelae (6), not resolved (49) and unknown (42). Conclusion: This cumulative case review does not raise new safety issues. Surveillance will continue. |
| Stroke Search criteria: HLT Central nervous system haemorrhages and cerebrovascular accidents | Number of cases: 275 (0.6% of the total PM dataset), of which 180 medically confirmed and 95 non-medically confirmed;Country of incidence: UK (81), US (66), France (32), Germany (21), Norway (14), Netherlands and Spain (11 each), Sweden (9), |
| AESIsa Category | Post-Marketing Cases Evaluationb Total Number of Cases (N=42086) |
| (Primary Path) OR HLT Cerebrovascular venous and sinus thrombosis (Primary Path) | Israel (6), Italy (5), Belgium (3), Denmark, Finland, Poland and Switzerland (2 each); the remaining 8 cases originated from 8 different countries; Subjects’ gender (n= 273): female (182), male (91);Subjects’ age group (n=265): Adult (59), Elderly (205), Childm (1);Number of relevant events: 300, all serious;Most frequently reported relevant PTs (>1 occurrence) included:PTs indicative of Ischaemic stroke: Cerebrovascular accident (160), Ischaemic stroke (41), Cerebral infarction (15), Cerebral ischaemia, Cerebral thrombosis, Cerebral venous sinus thrombosis, Ischaemic cerebral infarction and Lacunal infarction (3 each) Basal ganglia stroke, Cerebellar infarction and Thrombotic stroke (2 each);PTs indicative of Haemorrhagic stroke: Cerebral haemorrhage (26), Haemorrhagic stroke (11), Haemorrhage intracranical and Subarachnoid haemorrhage (5 each), Cerebral haematoma (4), Basal ganglia haemorrhage and Cerebellar haemorrhage (2 each);Relevant event onset latency (n = 241): Range from <24 hours to 41 days, median 2 days;Relevant event outcome: fatal and resolved/resolving (61 each), resolved with sequelae (10), not resolved (85) and unknown (83). Conclusion: This cumulative case review does not raise new safety issues. Surveillance will continue. |
| Vasculitic Events Search criteria: Vasculitides HLT | Number of cases: 32 cases (0.08% of the total PM dataset), of which 26 medically confirmed and 6 non-medically confirmed;Country of incidence: UK (13), France (4), Portugal, US and Spain (3 each), Cyprus, Germany, Hungary, Italy and Slovakia and Costa rica (1 each);Subjects’ gender: female (26), male (6);Subjects’ age group (n=31): Adult (15), Elderly (16);Number of relevant events: 34, of which 25 serious, 9 non-serious;Reported relevant PTs: Vasculitis (14), Cutaneous vasculitis and Vasculitic rash (4 each), (3), Giant cell arteritis and Peripheral ischaemia (3 each), Behcet’s syndrome and Hypersensitivity vasculitis (2 each) Palpable purpura, and Takayasu’s arteritis (1 each);Relevant event onset latency (n = 25): Range from <24 hours to 19 days, median 3 days;Relevant event outcome: fatal (1), resolved/resolving (13), not resolved (12) and unknown (8). Conclusion: This cumulative case review does not raise new safety issues. Surveillance will continue |
| AESIsa Category | Post-Marketing Cases Evaluationb Total Number of Cases (N=42086) |
- For the complete list of the AESIs, please refer to Appendix 5;
- Please note that this corresponds to evidence from post-EUA/conditional marketing authorisation approval data sources;
- Subjects with age ranged between 18 and 64 years;
- Subjects with age equal to or above 65 years;
- Subjects with age ranged between 2 and 11 years;
- Subjects with age ranged between 12 and less than 18 years;
- Multiple episodes of the same PT event were reported with a different clinical outcome within some cases hence the sum of the events outcome exceeds the total number of PT events;
- Subjects with age ranged between 1 (28 days) and 23 months;
- Twenty-four additional cases were excluded from the analysis as they were not cases of peripheral facial nerve palsy because they described other disorders (stroke, cerebral haemorrhage or transient ischaemic attack); 1 case was excluded from the analysis because it was invalid due to an unidentifiable reporter;
- This UK case report received from the UK MHRA described a 1-year-old subject who received the vaccine, and had left postauricular ear pain that progressed to left-sided Bell’s palsy 1 day following vaccination that had not resolved at the time of the report;
- If a case included both PT Facial paresis and PT Facial paralysis, only the PT Facial paralysis was considered in the descriptions of the events as it is most clinically important;
- Multiple episodes of the same PT event were reported with a different clinical outcome within some cases hence the sum of the events outcome exceeds the total number of PT events
- This UK case report received from the UK MHRA described a 7-year-old female subject who received the vaccine and had stroke (unknown outcome); no follow-up is possible for clarification.
- This PT not included in the AESIs/TME list was included in the review as relevant for ACCESS protocol criteria;
3.1.4. Medication error
Cases potentially indicative of medication errors1 that cumulatively occurred are summarized below.
- Number of relevant medication error cases: 20562 (4.9%) of which 1569 (3.7%) are medically confirmed.
- Number of relevant events: 2792
- Top 10 countries of incidence:
− US (1201), France (171), UK (138), Germany (88), Czech Republic (87), Sweden (49), Israel (45), Italy (42), Canada (35), Romania (33), Finland (21), Portugal (20), Norway (14), Puerto Rico (13), Poland (12), Austria and Spain (10 each).
Medication error case outcomes:
- Fatal (7)3,
- Recovered/recovering (354, of which 4 are serious),
- Recovered with sequelae (8, of which 3 serious)
1 MedDRA (version 23.1) Higher Level Terms: Accidental exposures to product; Product administration errors and issues; Product confusion errors and issues; Product dispensing errors and issues; Product label issues; Product monitoring errors and issues; Product preparation errors and issues; Product selection errors and issues; Product storage errors and issues in the product use system; Product transcribing errors and communication issues, OR Preferred Terms: Accidental poisoning; Circumstance or information capable of leading to device use error; Circumstance or information capable of leading to medication error; Contraindicated device used; Deprescribing error; Device use error; Dose calculation error; Drug titration error; Expired device used; Exposure via direct contact; Exposure via eye contact; Exposure via mucosa; Exposure via skin contact; Failure of child resistant product closure; Inadequate aseptic technique in use of product; Incorrect disposal of product; Intercepted medication error; Intercepted product prescribing error; Medication error; Multiple use of single-use product; Product advertising issue; Product distribution issue; Product prescribing error; Product prescribing issue; Product substitution error; Product temperature excursion issue; Product use in unapproved therapeutic environment; Radiation underdose; Underdose; Unintentional medical device removal; Unintentional use for unapproved indication; Vaccination error; Wrong device used; Wrong dosage form; Wrong dosage formulation; Wrong dose; Wrong drug; Wrong patient; Wrong product procured; Wrong product stored; Wrong rate; Wrong route; Wrong schedule; Wrong strength; Wrong technique in device usage process; Wrong technique in product usage process.
2 Thirty-five (35) cases were exclude from the analysis because describing medication errors occurring in an unspecified number of individuals or describing medication errors occurring with co suspects were determined to be non-contributory.
3 All the medication errors reported in these cases were assessed as non-serious occurrences with an unknown outcome; based on the available information including the causes of death, the relationship between the medication error and the death is weak. .
- Not recovered (189, of which 84 are serious),
- Unknown (1498, of which 33 are serious).
1371 cases reported only MEs without any associated clinical adverse event. The PTs most frequently reported (≥12 occurrences) were: Poor quality product administered (539), Product temperature excursion issue (253), Inappropriate schedule of product administration (225), Product preparation error (206), Underdose (202), Circumstance or information capable of leading to medication error (120), Product preparation issue (119), Wrong technique in product usage process (76), Incorrect route of product administration (66), Accidental overdose (33), Product administered at inappropriate site (27), Incorrect dose administered and Accidental exposure to the product (25 each), Exposure via skin contact (22), Wrong product administered (17), Incomplete course of vaccination, and Product administration error (14 each) Product administered to patient of inappropriate age (12).
In 685 cases, there were co-reported AEs. The most frequently co- associated AEs (˃ 40 occurrences) were: Headache (187), Pyrexia (161), Fatigue (135), Chills (127), Pain (107),
Vaccination site pain (100), Nausea (89), Myalgia (88), Pain in extremity (85) Arthralgia
(68), Off label use (57), Dizziness (52), Lymphadenopathy (47), Asthenia (46) and Malaise (41). These cases are summarized in Table 8.
Table 8. ME PTs by seriousness with or without harm co-association (Through 28 February 2021)
| Serious | Non-Serious | |||
| ME PTs | With Harm | Without Harm | With Harm | Without Harm |
| Accidental exposure to product | 0 | 0 | 0 | 5 |
| Accidental overdose | 4 | 1 | 9 | 6 |
| Booster dose missed | 0 | 0 | 0 | 1 |
| Circumstance or information capable of leading to medication error | 0 | 0 | 5 | 11 |
| Contraindicated product administered | 1 | 0 | 0 | 2 |
| Expired product administered | 0 | 0 | 0 | 2 |
| Exposure via skin contact | 0 | 0 | 0 | 5 |
| Inappropriate schedule of product administration | 0 | 2 | 8 | 264 |
| Incorrect dose administered | 1 | 1 | 0 | 0 |
Table 8. ME PTs by seriousness with or without harm co-association (Through 28 February 2021)
| Serious | Non-Serious | |||
| ME PTs | With Harm | Without Harm | With Harm | Without Harm |
| Incorrect route of product administration | 2 | 6 | 16 | 127 |
| Lack of vaccination site rotation | 1 | 0 | 0 | 0 |
| Medication error | 0 | 0 | 0 | 1 |
| Poor quality product administered | 1 | 0 | 0 | 34 |
| Product administered at inappropriate site | 2 | 1 | 13 | 29 |
| Product administered to patient of inappropriate age | 0 | 4 | 0 | 40 |
| Product administration error | 1 | 0 | 0 | 3 |
| Product dose omission issue | 0 | 1 | 0 | 3 |
| Product preparation error | 1 | 0 | 4 | 11 |
| Product preparation issue | 1 | 1 | 0 | 14 |
Overall, there were 68 cases with co-reported AEs reporting Harm and 599 cases with co- reported AEs without harm. Additionally, Intercepted medication errors was reported in 1 case (PTs Malaise, clinical outcome unknow) and Potential medication errors were reported in 17 cases.
4. DISCUSSION
Pfizer performs frequent and rigorous signal detection on BNT162b2 cases. The findings of these signal detection analyses are consistent with the known safety profile of the vaccine.
This cumulative analysis to support the Biologics License Application for BNT162b2, is an integrated analysis of post-authorization safety data, from U.S. and foreign experience, focused on Important Identified Risks, Important Potential Risks, and areas of Important Missing Information identified in the Pharmacovigilance Plan, as well as adverse events of special interest and vaccine administration errors (whether or not associated with an adverse event). The data do not reveal any novel safety concerns or risks requiring label changes and support a favorable benefit risk profile of to the BNT162b2 vaccine.
5. SUMMARY AND CONCLUSION
Review of the available data for this cumulative PM experience, confirms a favorable benefit: risk balance for BNT162b2.
Pfizer will continue routine pharmacovigilance activities on behalf of BioNTech according to the Pharmacovigilance Agreement in place, in order to assure patient safety and will inform the Agency if an evaluation of the safety data yields significant new information for BNT162b2.
5.3.6 Cumulative Analysis of Post-authorization Adverse Event Reports
APPENDIX 1. LIST OF ADVERSE EVENTS OF SPECIAL INTEREST
1p36 deletion syndrome;2-Hydroxyglutaric aciduria;5’nucleotidase increased;Acoustic neuritis;Acquired C1 inhibitor deficiency;Acquired epidermolysis bullosa;Acquired epileptic aphasia;Acute cutaneous lupus erythematosus;Acute disseminated encephalomyelitis;Acute encephalitis with refractory, repetitive partial seizures;Acute febrile neutrophilic dermatosis;Acute flaccid myelitis;Acute haemorrhagic leukoencephalitis;Acute haemorrhagic oedema of infancy;Acute kidney injury;Acute macular outer retinopathy;Acute motor axonal neuropathy;Acute motor-sensory axonal neuropathy;Acute myocardial infarction;Acute respiratory distress syndrome;Acute respiratory failure;Addison’s disease;Administration site thrombosis;Administration site vasculitis;Adrenal thrombosis;Adverse event following immunisation;Ageusia;Agranulocytosis;Air embolism;Alanine aminotransferase abnormal;Alanine aminotransferase increased;Alcoholic seizure;Allergic bronchopulmonary mycosis;Allergic oedema;Alloimmune hepatitis;Alopecia areata;Alpers disease;Alveolar proteinosis;Ammonia abnormal;Ammonia increased;Amniotic cavity infection;Amygdalohippocampectomy;Amyloid arthropathy;Amyloidosis;Amyloidosis senile;Anaphylactic reaction;Anaphylactic shock;Anaphylactic transfusion reaction;Anaphylactoid reaction;Anaphylactoid shock;Anaphylactoid syndrome of pregnancy;Angioedema;Angiopathic neuropathy;Ankylosing spondylitis;Anosmia;Antiacetylcholine receptor antibody positive;Anti-actin antibody positive;Anti-aquaporin-4 antibody positive;Anti-basal ganglia antibody positive;Anti-cyclic citrullinated peptide antibody positive;Anti-epithelial antibody positive;Anti-erythrocyte antibody positive;Anti-exosome complex antibody positive;Anti- GAD antibody negative;Anti-GAD antibody positive;Anti-ganglioside antibody positive;Antigliadin antibody positive;Anti-glomerular basement membrane antibody positive;Anti-glomerular basement membrane disease;Anti-glycyl-tRNA synthetase antibody positive;Anti-HLA antibody test positive;Anti-IA2 antibody positive;Anti-insulin antibody increased;Anti-insulin antibody positive;Anti-insulin receptor antibody increased;Anti- insulin receptor antibody positive;Anti-interferon antibody negative;Anti-interferon antibody positive;Anti-islet cell antibody positive;Antimitochondrial antibody positive;Anti-muscle specific kinase antibody positive;Anti-myelin-associated glycoprotein antibodies positive;Anti-myelin-associated glycoprotein associated polyneuropathy;Antimyocardial antibody positive;Anti-neuronal antibody positive;Antineutrophil cytoplasmic antibody increased;Antineutrophil cytoplasmic antibody positive;Anti-neutrophil cytoplasmic antibody positive vasculitis;Anti-NMDA antibody positive;Antinuclear antibody increased;Antinuclear antibody positive;Antiphospholipid antibodies positive;Antiphospholipid syndrome;Anti-platelet antibody positive;Anti-prothrombin antibody positive;Antiribosomal P antibody positive;Anti-RNA polymerase III antibody positive;Anti-saccharomyces cerevisiae antibody test positive;Anti-sperm antibody positive;Anti-SRP antibody positive;Antisynthetase syndrome;Anti-thyroid antibody positive;Anti-transglutaminase antibody increased;Anti-VGCC antibody positive;Anti- VGKC antibody positive;Anti-vimentin antibody positive;Antiviral prophylaxis;Antiviral treatment;Anti-zinc transporter 8 antibody positive;Aortic embolus;Aortic thrombosis;Aortitis;Aplasia pure red cell;Aplastic anaemia;Application site thrombosis;Application site vasculitis;Arrhythmia;Arterial bypass occlusion;Arterial bypass thrombosis;Arterial thrombosis;Arteriovenous fistula thrombosis;Arteriovenous graft site stenosis;Arteriovenous graft thrombosis;Arteritis;Arteritis
5.3.6 Cumulative Analysis of Post-authorization Adverse Event Reports
coronary;Arthralgia;Arthritis;Arthritis enteropathic;Ascites;Aseptic cavernous sinus thrombosis;Aspartate aminotransferase abnormal;Aspartate aminotransferase increased;Aspartate-glutamate-transporter deficiency;AST to platelet ratio index increased;AST/ALT ratio abnormal;Asthma;Asymptomatic COVID- 19;Ataxia;Atheroembolism;Atonic seizures;Atrial thrombosis;Atrophic thyroiditis;Atypical benign partial epilepsy;Atypical pneumonia;Aura;Autoantibody positive;Autoimmune anaemia;Autoimmune aplastic anaemia;Autoimmune arthritis;Autoimmune blistering disease;Autoimmune cholangitis;Autoimmune colitis;Autoimmune demyelinating disease;Autoimmune dermatitis;Autoimmune disorder;Autoimmune encephalopathy;Autoimmune endocrine disorder;Autoimmune enteropathy;Autoimmune eye disorder;Autoimmune haemolytic anaemia;Autoimmune heparin-induced thrombocytopenia;Autoimmune hepatitis;Autoimmune hyperlipidaemia;Autoimmune hypothyroidism;Autoimmune inner ear disease;Autoimmune lung disease;Autoimmune lymphoproliferative syndrome;Autoimmune myocarditis;Autoimmune myositis;Autoimmune nephritis;Autoimmune neuropathy;Autoimmune neutropenia;Autoimmune pancreatitis;Autoimmune pancytopenia;Autoimmune pericarditis;Autoimmune retinopathy;Autoimmune thyroid disorder;Autoimmune thyroiditis;Autoimmune uveitis;Autoinflammation with infantile enterocolitis;Autoinflammatory disease;Automatism epileptic;Autonomic nervous system imbalance;Autonomic seizure;Axial spondyloarthritis;Axillary vein thrombosis;Axonal and demyelinating polyneuropathy;Axonal neuropathy;Bacterascites;Baltic myoclonic epilepsy;Band sensation;Basedow’s disease;Basilar artery thrombosis;Basophilopenia;B-cell aplasia;Behcet’s syndrome;Benign ethnic neutropenia;Benign familial neonatal convulsions;Benign familial pemphigus;Benign rolandic epilepsy;Beta-2 glycoprotein antibody positive;Bickerstaff’s encephalitis;Bile output abnormal;Bile output decreased;Biliary ascites;Bilirubin conjugated abnormal;Bilirubin conjugated increased;Bilirubin urine present;Biopsy liver abnormal;Biotinidase deficiency;Birdshot chorioretinopathy;Blood alkaline phosphatase abnormal;Blood alkaline phosphatase increased;Blood bilirubin abnormal;Blood bilirubin increased;Blood bilirubin unconjugated increased;Blood cholinesterase abnormal;Blood cholinesterase decreased;Blood pressure decreased;Blood pressure diastolic decreased;Blood pressure systolic decreased;Blue toe syndrome;Brachiocephalic vein thrombosis;Brain stem embolism;Brain stem thrombosis;Bromosulphthalein test abnormal;Bronchial oedema;Bronchitis;Bronchitis mycoplasmal;Bronchitis viral;Bronchopulmonary aspergillosis allergic;Bronchospasm;Budd- Chiari syndrome;Bulbar palsy;Butterfly rash;C1q nephropathy;Caesarean section;Calcium embolism;Capillaritis;Caplan’s syndrome;Cardiac amyloidosis;Cardiac arrest;Cardiac failure;Cardiac failure acute;Cardiac sarcoidosis;Cardiac ventricular thrombosis;Cardiogenic shock;Cardiolipin antibody positive;Cardiopulmonary failure;Cardio-respiratory arrest;Cardio-respiratory distress;Cardiovascular insufficiency;Carotid arterial embolus;Carotid artery thrombosis;Cataplexy;Catheter site thrombosis;Catheter site vasculitis;Cavernous sinus thrombosis;CDKL5 deficiency disorder;CEC syndrome;Cement embolism;Central nervous system lupus;Central nervous system vasculitis;Cerebellar artery thrombosis;Cerebellar embolism;Cerebral amyloid angiopathy;Cerebral arteritis;Cerebral artery embolism;Cerebral artery thrombosis;Cerebral gas embolism;Cerebral microembolism;Cerebral septic infarct;Cerebral thrombosis;Cerebral venous sinus thrombosis;Cerebral venous thrombosis;Cerebrospinal thrombotic
5.3.6 Cumulative Analysis of Post-authorization Adverse Event Reports
tamponade;Cerebrovascular accident;Change in seizure presentation;Chest discomfort;Child- Pugh-Turcotte score abnormal;Child-Pugh-Turcotte score increased;Chillblains;Choking;Choking sensation;Cholangitis sclerosing;Chronic autoimmune glomerulonephritis;Chronic cutaneous lupus erythematosus;Chronic fatigue syndrome;Chronic gastritis;Chronic inflammatory demyelinating polyradiculoneuropathy;Chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids;Chronic recurrent multifocal osteomyelitis;Chronic respiratory failure;Chronic spontaneous urticaria;Circulatory collapse;Circumoral oedema;Circumoral swelling;Clinically isolated syndrome;Clonic convulsion;Coeliac disease;Cogan’s syndrome;Cold agglutinins positive;Cold type haemolytic anaemia;Colitis;Colitis erosive;Colitis herpes;Colitis microscopic;Colitis ulcerative;Collagen disorder;Collagen-vascular disease;Complement factor abnormal;Complement factor C1 decreased;Complement factor C2 decreased;Complement factor C3 decreased;Complement factor C4 decreased;Complement factor decreased;Computerised tomogram liver abnormal;Concentric sclerosis;Congenital anomaly;Congenital bilateral perisylvian syndrome;Congenital herpes simplex infection;Congenital myasthenic syndrome;Congenital varicella infection;Congestive hepatopathy;Convulsion in childhood;Convulsions local;Convulsive threshold lowered;Coombs positive haemolytic anaemia;Coronary artery disease;Coronary artery embolism;Coronary artery thrombosis;Coronary bypass thrombosis;Coronavirus infection;Coronavirus test;Coronavirus test negative;Coronavirus test positive;Corpus callosotomy;Cough;Cough variant asthma;COVID-19;COVID-19 immunisation;COVID-19 pneumonia;COVID-19 prophylaxis;COVID-19 treatment;Cranial nerve disorder;Cranial nerve palsies multiple;Cranial nerve paralysis;CREST syndrome;Crohn’s disease;Cryofibrinogenaemia;Cryoglobulinaemia;CSF oligoclonal band present;CSWS syndrome;Cutaneous amyloidosis;Cutaneous lupus erythematosus;Cutaneous sarcoidosis;Cutaneous vasculitis;Cyanosis;Cyclic neutropenia;Cystitis interstitial;Cytokine release syndrome;Cytokine storm;De novo purine synthesis inhibitors associated acute inflammatory syndrome;Death neonatal;Deep vein thrombosis;Deep vein thrombosis postoperative;Deficiency of bile secretion;Deja vu;Demyelinating polyneuropathy;Demyelination;Dermatitis;Dermatitis bullous;Dermatitis herpetiformis;Dermatomyositis;Device embolisation;Device related thrombosis;Diabetes mellitus;Diabetic ketoacidosis;Diabetic mastopathy;Dialysis amyloidosis;Dialysis membrane reaction;Diastolic hypotension;Diffuse vasculitis;Digital pitting scar;Disseminated intravascular coagulation;Disseminated intravascular coagulation in newborn;Disseminated neonatal herpes simplex;Disseminated varicella;Disseminated varicella zoster vaccine virus infection;Disseminated varicella zoster virus infection;DNA antibody positive;Double cortex syndrome;Double stranded DNA antibody positive;Dreamy state;Dressler’s syndrome;Drop attacks;Drug withdrawal convulsions;Dyspnoea;Early infantile epileptic encephalopathy with burst-suppression;Eclampsia;Eczema herpeticum;Embolia cutis medicamentosa;Embolic cerebellar infarction;Embolic cerebral infarction;Embolic pneumonia;Embolic stroke;Embolism;Embolism arterial;Embolism venous;Encephalitis;Encephalitis allergic;Encephalitis autoimmune;Encephalitis brain stem;Encephalitis haemorrhagic;Encephalitis periaxialis diffusa;Encephalitis post immunisation;Encephalomyelitis;Encephalopathy;Endocrine disorder;Endocrine ophthalmopathy;Endotracheal intubation;Enteritis;Enteritis leukopenic;Enterobacter pneumonia;Enterocolitis;Enteropathic spondylitis;Eosinopenia;Eosinophilic
5.3.6 Cumulative Analysis of Post-authorization Adverse Event Reports
fasciitis;Eosinophilic granulomatosis with polyangiitis;Eosinophilic oesophagitis;Epidermolysis;Epilepsy;Epilepsy surgery;Epilepsy with myoclonic-atonic seizures;Epileptic aura;Epileptic psychosis;Erythema;Erythema induratum;Erythema multiforme;Erythema nodosum;Evans syndrome;Exanthema subitum;Expanded disability status scale score decreased;Expanded disability status scale score increased;Exposure to communicable disease;Exposure to SARS-CoV-2;Eye oedema;Eye pruritus;Eye swelling;Eyelid oedema;Face oedema;Facial paralysis;Facial paresis;Faciobrachial dystonic seizure;Fat embolism;Febrile convulsion;Febrile infection-related epilepsy syndrome;Febrile neutropenia;Felty’s syndrome;Femoral artery embolism;Fibrillary glomerulonephritis;Fibromyalgia;Flushing;Foaming at mouth;Focal cortical resection;Focal dyscognitive seizures;Foetal distress syndrome;Foetal placental thrombosis;Foetor hepaticus;Foreign body embolism;Frontal lobe epilepsy;Fulminant type 1 diabetes mellitus;Galactose elimination capacity test abnormal;Galactose elimination capacity test decreased;Gamma-glutamyltransferase abnormal;Gamma-glutamyltransferase increased;Gastritis herpes;Gastrointestinal amyloidosis;Gelastic seizure;Generalised onset non-motor seizure;Generalised tonic-clonic seizure;Genital herpes;Genital herpes simplex;Genital herpes zoster;Giant cell arteritis;Glomerulonephritis;Glomerulonephritis membranoproliferative;Glomerulonephritis membranous;Glomerulonephritis rapidly progressive;Glossopharyngeal nerve paralysis;Glucose transporter type 1 deficiency syndrome;Glutamate dehydrogenase increased;Glycocholic acid increased;GM2 gangliosidosis;Goodpasture’s syndrome;Graft thrombosis;Granulocytopenia;Granulocytopenia neonatal;Granulomatosis with polyangiitis;Granulomatous dermatitis;Grey matter heterotopia;Guanase increased;Guillain- Barre syndrome;Haemolytic anaemia;Haemophagocytic lymphohistiocytosis;Haemorrhage;Haemorrhagic ascites;Haemorrhagic disorder;Haemorrhagic pneumonia;Haemorrhagic varicella syndrome;Haemorrhagic vasculitis;Hantavirus pulmonary infection;Hashimoto’s encephalopathy;Hashitoxicosis;Hemimegalencephaly;Henoch-Schonlein purpura;Henoch- Schonlein purpura nephritis;Hepaplastin abnormal;Hepaplastin decreased;Heparin-induced thrombocytopenia;Hepatic amyloidosis;Hepatic artery embolism;Hepatic artery flow decreased;Hepatic artery thrombosis;Hepatic enzyme abnormal;Hepatic enzyme decreased;Hepatic enzyme increased;Hepatic fibrosis marker abnormal;Hepatic fibrosis marker increased;Hepatic function abnormal;Hepatic hydrothorax;Hepatic hypertrophy;Hepatic hypoperfusion;Hepatic lymphocytic infiltration;Hepatic mass;Hepatic pain;Hepatic sequestration;Hepatic vascular resistance increased;Hepatic vascular thrombosis;Hepatic vein embolism;Hepatic vein thrombosis;Hepatic venous pressure gradient abnormal;Hepatic venous pressure gradient increased;Hepatitis;Hepatobiliary scan abnormal;Hepatomegaly;Hepatosplenomegaly;Hereditary angioedema with C1 esterase inhibitor deficiency;Herpes dermatitis;Herpes gestationis;Herpes oesophagitis;Herpes ophthalmic;Herpes pharyngitis;Herpes sepsis;Herpes simplex;Herpes simplex cervicitis;Herpes simplex colitis;Herpes simplex encephalitis;Herpes simplex gastritis;Herpes simplex hepatitis;Herpes simplex meningitis;Herpes simplex meningoencephalitis;Herpes simplex meningomyelitis;Herpes simplex necrotising retinopathy;Herpes simplex oesophagitis;Herpes simplex otitis externa;Herpes simplex pharyngitis;Herpes simplex pneumonia;Herpes simplex reactivation;Herpes simplex sepsis;Herpes simplex viraemia;Herpes simplex virus conjunctivitis neonatal;Herpes simplex visceral;Herpes virus
5.3.6 Cumulative Analysis of Post-authorization Adverse Event Reports
infection;Herpes zoster;Herpes zoster cutaneous disseminated;Herpes zoster infection neurological;Herpes zoster meningitis;Herpes zoster meningoencephalitis;Herpes zoster meningomyelitis;Herpes zoster meningoradiculitis;Herpes zoster necrotising retinopathy;Herpes zoster oticus;Herpes zoster pharyngitis;Herpes zoster reactivation;Herpetic radiculopathy;Histone antibody positive;Hoigne’s syndrome;Human herpesvirus 6 encephalitis;Human herpesvirus 6 infection;Human herpesvirus 6 infection
reactivation;Human herpesvirus 7 infection;Human herpesvirus 8 infection;Hyperammonaemia;Hyperbilirubinaemia;Hypercholia;Hypergammaglobulinaemia benign monoclonal;Hyperglycaemic seizure;Hypersensitivity;Hypersensitivity vasculitis;Hyperthyroidism;Hypertransaminasaemia;Hyperventilation;Hypoalbuminaemia;H ypocalcaemic seizure;Hypogammaglobulinaemia;Hypoglossal nerve paralysis;Hypoglossal nerve paresis;Hypoglycaemic seizure;Hyponatraemic seizure;Hypotension;Hypotensive crisis;Hypothenar hammer syndrome;Hypothyroidism;Hypoxia;Idiopathic CD4 lymphocytopenia;Idiopathic generalised epilepsy;Idiopathic interstitial pneumonia;Idiopathic neutropenia;Idiopathic pulmonary fibrosis;IgA nephropathy;IgM nephropathy;IIIrd nerve paralysis;IIIrd nerve paresis;Iliac artery embolism;Immune thrombocytopenia;Immune- mediated adverse reaction;Immune-mediated cholangitis;Immune-mediated cholestasis;Immune-mediated cytopenia;Immune-mediated encephalitis;Immune-mediated encephalopathy;Immune-mediated endocrinopathy;Immune-mediated enterocolitis;Immune- mediated gastritis;Immune-mediated hepatic disorder;Immune-mediated hepatitis;Immune- mediated hyperthyroidism;Immune-mediated hypothyroidism;Immune-mediated myocarditis;Immune-mediated myositis;Immune-mediated nephritis;Immune-mediated neuropathy;Immune-mediated pancreatitis;Immune-mediated pneumonitis;Immune-mediated renal disorder;Immune-mediated thyroiditis;Immune-mediated uveitis;Immunoglobulin G4 related disease;Immunoglobulins abnormal;Implant site thrombosis;Inclusion body myositis;Infantile genetic agranulocytosis;Infantile spasms;Infected vasculitis;Infective thrombosis;Inflammation;Inflammatory bowel disease;Infusion site thrombosis;Infusion site vasculitis;Injection site thrombosis;Injection site urticaria;Injection site vasculitis;Instillation site thrombosis;Insulin autoimmune syndrome;Interstitial granulomatous dermatitis;Interstitial lung disease;Intracardiac mass;Intracardiac thrombus;Intracranial pressure increased;Intrapericardial thrombosis;Intrinsic factor antibody abnormal;Intrinsic factor antibody positive;IPEX syndrome;Irregular breathing;IRVAN syndrome;IVth nerve paralysis;IVth nerve paresis;JC polyomavirus test positive;JC virus CSF test positive;Jeavons syndrome;Jugular vein embolism;Jugular vein thrombosis;Juvenile idiopathic arthritis;Juvenile myoclonic epilepsy;Juvenile polymyositis;Juvenile psoriatic arthritis;Juvenile spondyloarthritis;Kaposi sarcoma inflammatory cytokine syndrome;Kawasaki’s disease;Kayser-Fleischer ring;Keratoderma blenorrhagica;Ketosis- prone diabetes mellitus;Kounis syndrome;Lafora’s myoclonic epilepsy;Lambl’s excrescences;Laryngeal dyspnoea;Laryngeal oedema;Laryngeal rheumatoid arthritis;Laryngospasm;Laryngotracheal oedema;Latent autoimmune diabetes in adults;LE cells present;Lemierre syndrome;Lennox-Gastaut syndrome;Leucine aminopeptidase increased;Leukoencephalomyelitis;Leukoencephalopathy;Leukopenia;Leukopenia neonatal;Lewis-Sumner syndrome;Lhermitte’s sign;Lichen planopilaris;Lichen planus;Lichen sclerosus;Limbic encephalitis;Linear IgA disease;Lip oedema;Lip swelling;Liver function test abnormal;Liver function test decreased;Liver function test increased;Liver induration;Liver injury;Liver iron concentration abnormal;Liver iron concentration
5.3.6 Cumulative Analysis of Post-authorization Adverse Event Reports
increased;Liver opacity;Liver palpable;Liver sarcoidosis;Liver scan abnormal;Liver tenderness;Low birth weight baby;Lower respiratory tract herpes infection;Lower respiratory tract infection;Lower respiratory tract infection viral;Lung abscess;Lupoid hepatic cirrhosis;Lupus cystitis;Lupus encephalitis;Lupus endocarditis;Lupus enteritis;Lupus hepatitis;Lupus myocarditis;Lupus myositis;Lupus nephritis;Lupus pancreatitis;Lupus pleurisy;Lupus pneumonitis;Lupus vasculitis;Lupus-like syndrome;Lymphocytic hypophysitis;Lymphocytopenia neonatal;Lymphopenia;MAGIC syndrome;Magnetic resonance imaging liver abnormal;Magnetic resonance proton density fat fraction measurement;Mahler sign;Manufacturing laboratory analytical testing issue;Manufacturing materials issue;Manufacturing production issue;Marburg’s variant multiple sclerosis;Marchiafava-Bignami disease;Marine Lenhart syndrome;Mastocytic enterocolitis;Maternal exposure during pregnancy;Medical device site thrombosis;Medical device site vasculitis;MELAS syndrome;Meningitis;Meningitis aseptic;Meningitis herpes;Meningoencephalitis herpes simplex neonatal;Meningoencephalitis herpetic;Meningomyelitis herpes;MERS-CoV test;MERS-CoV test negative;MERS-CoV test positive;Mesangioproliferative glomerulonephritis;Mesenteric artery embolism;Mesenteric artery thrombosis;Mesenteric vein thrombosis;Metapneumovirus infection;Metastatic cutaneous Crohn’s disease;Metastatic pulmonary embolism;Microangiopathy;Microembolism;Microscopic polyangiitis;Middle East respiratory syndrome;Migraine-triggered seizure;Miliary pneumonia;Miller Fisher syndrome;Mitochondrial aspartate aminotransferase increased;Mixed connective tissue disease;Model for end stage liver disease score abnormal;Model for end stage liver disease score increased;Molar ratio of total branched-chain amino acid to tyrosine;Molybdenum cofactor deficiency;Monocytopenia;Mononeuritis;Mononeuropathy multiplex;Morphoea;Morvan syndrome;Mouth swelling;Moyamoya disease;Multifocal motor neuropathy;Multiple organ dysfunction syndrome;Multiple sclerosis;Multiple sclerosis relapse;Multiple sclerosis relapse prophylaxis;Multiple subpial transection;Multisystem inflammatory syndrome in children;Muscular sarcoidosis;Myasthenia gravis;Myasthenia gravis crisis;Myasthenia gravis neonatal;Myasthenic syndrome;Myelitis;Myelitis transverse;Myocardial infarction;Myocarditis;Myocarditis post infection;Myoclonic epilepsy;Myoclonic epilepsy and ragged-red fibres;Myokymia;Myositis;Narcolepsy;Nasal herpes;Nasal obstruction;Necrotising herpetic retinopathy;Neonatal Crohn’s disease;Neonatal epileptic seizure;Neonatal lupus erythematosus;Neonatal mucocutaneous herpes simplex;Neonatal pneumonia;Neonatal seizure;Nephritis;Nephrogenic systemic fibrosis;Neuralgic amyotrophy;Neuritis;Neuritis cranial;Neuromyelitis optica pseudo relapse;Neuromyelitis optica spectrum disorder;Neuromyotonia;Neuronal neuropathy;Neuropathy peripheral;Neuropathy, ataxia, retinitis pigmentosa syndrome;Neuropsychiatric lupus;Neurosarcoidosis;Neutropenia;Neutropenia neonatal;Neutropenic colitis;Neutropenic infection;Neutropenic sepsis;Nodular rash;Nodular vasculitis;Noninfectious myelitis;Noninfective encephalitis;Noninfective encephalomyelitis;Noninfective oophoritis;Obstetrical pulmonary embolism;Occupational exposure to communicable disease;Occupational exposure to SARS-CoV-2;Ocular hyperaemia;Ocular myasthenia;Ocular pemphigoid;Ocular sarcoidosis;Ocular vasculitis;Oculofacial paralysis;Oedema;Oedema blister;Oedema due to hepatic disease;Oedema mouth;Oesophageal achalasia;Ophthalmic artery thrombosis;Ophthalmic herpes simplex;Ophthalmic herpes zoster;Ophthalmic vein thrombosis;Optic neuritis;Optic
5.3.6 Cumulative Analysis of Post-authorization Adverse Event Reports
neuropathy;Optic perineuritis;Oral herpes;Oral lichen planus;Oropharyngeal oedema;Oropharyngeal spasm;Oropharyngeal swelling;Osmotic demyelination syndrome;Ovarian vein thrombosis;Overlap syndrome;Paediatric autoimmune neuropsychiatric disorders associated with streptococcal infection;Paget-Schroetter syndrome;Palindromic rheumatism;Palisaded neutrophilic granulomatous dermatitis;Palmoplantar keratoderma;Palpable purpura;Pancreatitis;Panencephalitis;Papillophlebitis;Paracancerous pneumonia;Paradoxical embolism;Parainfluenzae viral laryngotracheobronchitis;Paraneoplastic dermatomyositis;Paraneoplastic pemphigus;Paraneoplastic thrombosis;Paresis cranial nerve;Parietal cell antibody positive;Paroxysmal nocturnal haemoglobinuria;Partial seizures;Partial seizures with secondary generalisation;Patient isolation;Pelvic venous thrombosis;Pemphigoid;Pemphigus;Penile vein thrombosis;Pericarditis;Pericarditis lupus;Perihepatic discomfort;Periorbital oedema;Periorbital swelling;Peripheral artery thrombosis;Peripheral embolism;Peripheral ischaemia;Peripheral vein thrombus extension;Periportal oedema;Peritoneal fluid protein abnormal;Peritoneal fluid protein decreased;Peritoneal fluid protein increased;Peritonitis lupus;Pernicious anaemia;Petit mal epilepsy;Pharyngeal oedema;Pharyngeal swelling;Pityriasis lichenoides et varioliformis acuta;Placenta praevia;Pleuroparenchymal fibroelastosis;Pneumobilia;Pneumonia;Pneumonia adenoviral;Pneumonia cytomegaloviral;Pneumonia herpes viral;Pneumonia influenzal;Pneumonia measles;Pneumonia mycoplasmal;Pneumonia necrotising;Pneumonia parainfluenzae viral;Pneumonia respiratory syncytial viral;Pneumonia viral;POEMS syndrome;Polyarteritis nodosa;Polyarthritis;Polychondritis;Polyglandular autoimmune syndrome type I;Polyglandular autoimmune syndrome type II;Polyglandular autoimmune syndrome type III;Polyglandular disorder;Polymicrogyria;Polymyalgia rheumatica;Polymyositis;Polyneuropathy;Polyneuropathy idiopathic progressive;Portal pyaemia;Portal vein embolism;Portal vein flow decreased;Portal vein pressure increased;Portal vein thrombosis;Portosplenomesenteric venous thrombosis;Post procedural hypotension;Post procedural pneumonia;Post procedural pulmonary embolism;Post stroke epilepsy;Post stroke seizure;Post thrombotic retinopathy;Post thrombotic syndrome;Post viral fatigue syndrome;Postictal headache;Postictal paralysis;Postictal psychosis;Postictal state;Postoperative respiratory distress;Postoperative respiratory failure;Postoperative thrombosis;Postpartum thrombosis;Postpartum venous thrombosis;Postpericardiotomy syndrome;Post-traumatic epilepsy;Postural orthostatic tachycardia syndrome;Precerebral artery thrombosis;Pre-eclampsia;Preictal state;Premature labour;Premature menopause;Primary amyloidosis;Primary biliary cholangitis;Primary progressive multiple sclerosis;Procedural shock;Proctitis herpes;Proctitis ulcerative;Product availability issue;Product distribution issue;Product supply issue;Progressive facial hemiatrophy;Progressive multifocal leukoencephalopathy;Progressive multiple sclerosis;Progressive relapsing multiple sclerosis;Prosthetic cardiac valve thrombosis;Pruritus;Pruritus allergic;Pseudovasculitis;Psoriasis;Psoriatic arthropathy;Pulmonary amyloidosis;Pulmonary artery thrombosis;Pulmonary embolism;Pulmonary fibrosis;Pulmonary haemorrhage;Pulmonary microemboli;Pulmonary oil microembolism;Pulmonary renal syndrome;Pulmonary sarcoidosis;Pulmonary sepsis;Pulmonary thrombosis;Pulmonary tumour thrombotic microangiopathy;Pulmonary vasculitis;Pulmonary veno-occlusive disease;Pulmonary venous thrombosis;Pyoderma gangrenosum;Pyostomatitis vegetans;Pyrexia;Quarantine;Radiation leukopenia;Radiculitis
5.3.6 Cumulative Analysis of Post-authorization Adverse Event Reports
brachial;Radiologically isolated syndrome;Rash;Rash erythematous;Rash pruritic;Rasmussen encephalitis;Raynaud’s phenomenon;Reactive capillary endothelial proliferation;Relapsing multiple sclerosis;Relapsing-remitting multiple sclerosis;Renal amyloidosis;Renal arteritis;Renal artery thrombosis;Renal embolism;Renal failure;Renal vascular thrombosis;Renal vasculitis;Renal vein embolism;Renal vein thrombosis;Respiratory arrest;Respiratory disorder;Respiratory distress;Respiratory failure;Respiratory paralysis;Respiratory syncytial virus bronchiolitis;Respiratory syncytial virus bronchitis;Retinal artery embolism;Retinal artery occlusion;Retinal artery thrombosis;Retinal vascular thrombosis;Retinal vasculitis;Retinal vein occlusion;Retinal vein thrombosis;Retinol binding protein decreased;Retinopathy;Retrograde portal vein flow;Retroperitoneal fibrosis;Reversible airways obstruction;Reynold’s syndrome;Rheumatic brain disease;Rheumatic disorder;Rheumatoid arthritis;Rheumatoid factor increased;Rheumatoid factor positive;Rheumatoid factor quantitative increased;Rheumatoid lung;Rheumatoid neutrophilic dermatosis;Rheumatoid nodule;Rheumatoid nodule removal;Rheumatoid scleritis;Rheumatoid vasculitis;Saccadic eye movement;SAPHO syndrome;Sarcoidosis;SARS-CoV-1 test;SARS-CoV-1 test negative;SARS-CoV-1 test positive;SARS-CoV-2 antibody test;SARS-CoV-2 antibody test negative;SARS-CoV-2 antibody test positive;SARS-CoV-2 carrier;SARS-CoV-2 sepsis;SARS-CoV-2 test;SARS- CoV-2 test false negative;SARS-CoV-2 test false positive;SARS-CoV-2 test negative;SARS- CoV-2 test positive;SARS-CoV-2 viraemia;Satoyoshi syndrome;Schizencephaly;Scleritis;Sclerodactylia;Scleroderma;Scleroderma associated digital ulcer;Scleroderma renal crisis;Scleroderma-like reaction;Secondary amyloidosis;Secondary cerebellar degeneration;Secondary progressive multiple sclerosis;Segmented hyalinising vasculitis;Seizure;Seizure anoxic;Seizure cluster;Seizure like phenomena;Seizure prophylaxis;Sensation of foreign body;Septic embolus;Septic pulmonary embolism;Severe acute respiratory syndrome;Severe myoclonic epilepsy of infancy;Shock;Shock symptom;Shrinking lung syndrome;Shunt thrombosis;Silent thyroiditis;Simple partial seizures;Sjogren’s syndrome;Skin swelling;SLE arthritis;Smooth muscle antibody positive;Sneezing;Spinal artery embolism;Spinal artery thrombosis;Splenic artery thrombosis;Splenic embolism;Splenic thrombosis;Splenic vein thrombosis;Spondylitis;Spondyloarthropathy;Spontaneous heparin-induced thrombocytopenia syndrome;Status epilepticus;Stevens-Johnson syndrome;Stiff leg syndrome;Stiff person syndrome;Stillbirth;Still’s disease;Stoma site thrombosis;Stoma site vasculitis;Stress cardiomyopathy;Stridor;Subacute cutaneous lupus erythematosus;Subacute endocarditis;Subacute inflammatory demyelinating polyneuropathy;Subclavian artery embolism;Subclavian artery thrombosis;Subclavian vein thrombosis;Sudden unexplained death in epilepsy;Superior sagittal sinus thrombosis;Susac’s syndrome;Suspected COVID- 19;Swelling;Swelling face;Swelling of eyelid;Swollen tongue;Sympathetic ophthalmia;Systemic lupus erythematosus;Systemic lupus erythematosus disease activity index abnormal;Systemic lupus erythematosus disease activity index decreased;Systemic lupus erythematosus disease activity index increased;Systemic lupus erythematosus rash;Systemic scleroderma;Systemic sclerosis pulmonary;Tachycardia;Tachypnoea;Takayasu’s arteritis;Temporal lobe epilepsy;Terminal ileitis;Testicular autoimmunity;Throat tightness;Thromboangiitis obliterans;Thrombocytopenia;Thrombocytopenic purpura;Thrombophlebitis;Thrombophlebitis migrans;Thrombophlebitis
5.3.6 Cumulative Analysis of Post-authorization Adverse Event Reports
neonatal;Thrombophlebitis septic;Thrombophlebitis superficial;Thromboplastin antibody positive;Thrombosis;Thrombosis corpora cavernosa;Thrombosis in device;Thrombosis mesenteric vessel;Thrombotic cerebral infarction;Thrombotic microangiopathy;Thrombotic stroke;Thrombotic thrombocytopenic purpura;Thyroid disorder;Thyroid stimulating immunoglobulin increased;Thyroiditis;Tongue amyloidosis;Tongue biting;Tongue oedema;Tonic clonic movements;Tonic convulsion;Tonic posturing;Topectomy;Total bile acids increased;Toxic epidermal necrolysis;Toxic leukoencephalopathy;Toxic oil syndrome;Tracheal obstruction;Tracheal oedema;Tracheobronchitis;Tracheobronchitis mycoplasmal;Tracheobronchitis viral;Transaminases abnormal;Transaminases increased;Transfusion-related alloimmune neutropenia;Transient epileptic amnesia;Transverse sinus thrombosis;Trigeminal nerve paresis;Trigeminal neuralgia;Trigeminal palsy;Truncus coeliacus thrombosis;Tuberous sclerosis complex;Tubulointerstitial nephritis and uveitis syndrome;Tumefactive multiple sclerosis;Tumour embolism;Tumour thrombosis;Type 1 diabetes mellitus;Type I hypersensitivity;Type III immune complex mediated reaction;Uhthoff’s phenomenon;Ulcerative keratitis;Ultrasound liver abnormal;Umbilical cord thrombosis;Uncinate fits;Undifferentiated connective tissue disease;Upper airway obstruction;Urine bilirubin increased;Urobilinogen urine decreased;Urobilinogen urine increased;Urticaria;Urticaria papular;Urticarial vasculitis;Uterine rupture;Uveitis;Vaccination site thrombosis;Vaccination site vasculitis;Vagus nerve paralysis;Varicella;Varicella keratitis;Varicella post vaccine;Varicella zoster gastritis;Varicella zoster oesophagitis;Varicella zoster pneumonia;Varicella zoster sepsis;Varicella zoster virus infection;Vasa praevia;Vascular graft thrombosis;Vascular pseudoaneurysm thrombosis;Vascular purpura;Vascular stent thrombosis;Vasculitic rash;Vasculitic ulcer;Vasculitis;Vasculitis gastrointestinal;Vasculitis necrotising;Vena cava embolism;Vena cava thrombosis;Venous intravasation;Venous recanalisation;Venous thrombosis;Venous thrombosis in pregnancy;Venous thrombosis limb;Venous thrombosis neonatal;Vertebral artery thrombosis;Vessel puncture site thrombosis;Visceral venous thrombosis;VIth nerve paralysis;VIth nerve paresis;Vitiligo;Vocal cord paralysis;Vocal cord paresis;Vogt-Koyanagi-Harada disease;Warm type haemolytic anaemia;Wheezing;White nipple sign;XIth nerve paralysis;X-ray hepatobiliary abnormal;Young’s syndrome;Zika virus associated Guillain Barre syndrome.











Mein Englisch ist leider eingerostet, wenn ich dann so einen langen englischen Fachtext sehe, rostet es gleich noch etwas mehr…
Gibt es die Studie nicht in deutsch? Wäre schön zur Aufklärung.
Vom Browser übersetzen lassen…
Hallo,
mit Google-Übersetzer kann man dies recht flüssig lesen.